WHO statement on mortality in Al Hol camp, Syria
22 September 2019 –The World Health Organization (WHO) has serious concerns over recent reporting of an increase in the number of child deaths in Al Hol camp. Such reporting has provided an inaccurate analysis on under-5 mortality, misrepresented some of the data, and overstated the gravity of the health situation in the camp.
While health needs in both the Annex – which houses foreign nationals - and the rest of the camp remain acute, overall mortality rates have been within international standards since April 2019; under-5 mortality rates have remained within international standards since May 2019. Contrary to the inaccurate reporting, there has been no increase in child deaths since March and mortality rates have remained stable over the past 6 months. Given the challenging operating environment and large health needs in Al Hol, these outcomes reflect well on the effectiveness of the collective humanitarian response in the camp.
The number of deaths reported decreased from 52 deaths during the week of 5–11 March, to 3 deaths during the week of 27–31 August. In total from 4 December 2018 to 31 August 2019, 406 deaths were registered in the camp, including 313 children (77%) under the age of 5. The high proportion of childhood deaths is largely due to the unusual demographics of the camp – the vast majority of residents are women and children – of which children under 5 currently represent 28.5% of the overall camp population.
WHO and health partners are working tirelessly to respond to health needs in Al Hol camp and have made significant efforts to scale up to the provision of health services.
Access to health care for camp residents is being progressively expanded, with 3 field hospitals, 18 static medical points, 8 mobile teams, 3 delivery clinics, 2 vaccination teams, and two family well-being centres providing services to the camp’s inhabitants. 12 medical points are reporting cases of infectious disease to the camp’s disease surveillance system.
WHO and partners will continue to work in a coordinated manner to further increase the range, coverage and quality of health services in the camp – and to avert all preventable deaths. Concerns regarding access to health care services in the Annex, as well as the high percentage of deaths in the community are shared by WHO and health partners, who are working vigorously to address these issues.
While continuing to expand access to humanitarian assistance is vital, WHO affirms that finding durable solutions for the residents of the camp must remain a major priority for the international community.
Iran floods leave people with limited access to life-saving health services

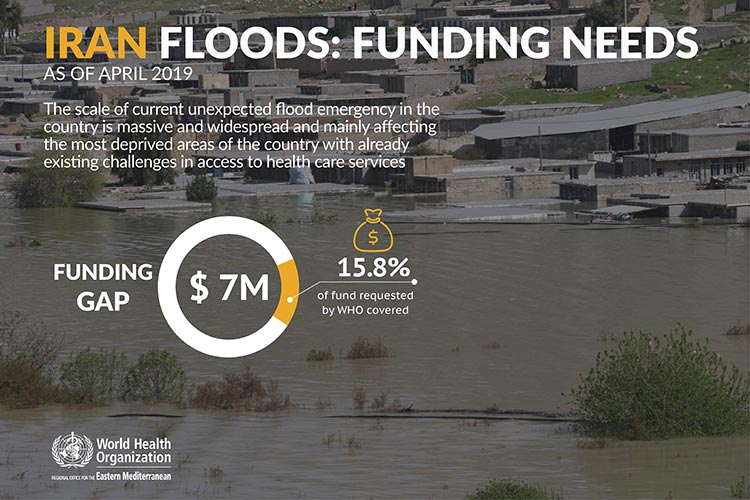
10 May 2019 - On 18 March 2019, a flood hit the eastern part of Mazandaran and Golestan provinces after four days of heavy rain. A few days later, additional floods in the west, southwest, and northeast of the country affected thousands of people. Shortly after, a third wave of heavy rains commenced.
As of 9 April, a total of 28 provinces have been affected by the floods (out of 31 provinces in total).
Overall, a total of 42 269 129 people have been affected by the floods across, almost 392,859 people have been displaced, 84 have died, and around 20,573 persons were injured.
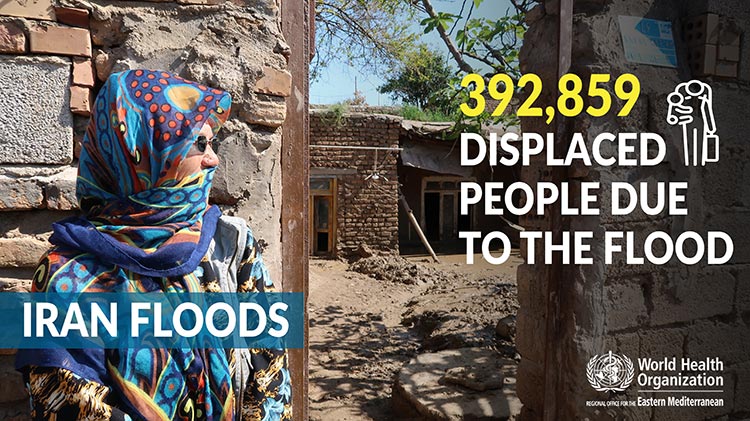
The total estimated population in need of immediate health care assistance is around 3,000,000 people.
People in need for health care assistance
People internally displaced due to the flood
Children affected in the most vulnerable areas
Health facilities damaged in the most affected areas
Provinces affected by the floods (out of 31 provinces)
Deaths (84) and injuries (20573) due to the floods
The floods have fully and partially destroyed 1040 health facilities and 81 hospitals, leaving patients with limited access to essential and life-saving health services.
In some provinces, health facilities are not functional due to inaccessibility due to road blocks, running water, and landslides as well as due to standing water in buildings.

Health workers are not able to reach populations in need, as transportation and infrastructure has been destroyed.
Dr Christoph Hamelmann - WHO Representative for the Islamic Republic of Iran
Related link
WHO and Federal Ministry of Health of Somalia call for urgent support to address measles outbreak in Somalia
16 August 2017 – As millions of people in Somalia remain trapped in a devastating cycle of hunger and disease, WHO and health partners are working with national health authorities to save lives and reach the most vulnerable with essential health services.
More than 2 years of insufficient rainfall and poor harvests have led to drought, food insecurity and a real risk of famine. Malnutrition, mass displacement as a result of the drought, and lack of access to clean water and sanitation have created ideal conditions for infectious disease outbreaks.
“Somalia is facing one of the worst humanitarian crises in the world. Millions of people, already on the brink of famine, are now at risk of rapidly spreading infectious diseases like cholera and measles. Normally, these diseases are easy to treat and prevent, but they can turn deadly when people are living in overcrowded spaces and are too weak to fight off infection,” said Dr Ghulam Popal, WHO Representative in Somalia.
Drought has led to a lack of clean water and the largest cholera outbreak in the last 5 years, with more than 57 000 cases and 809 cumulative deaths reported as of 31 July 2017. Health partners, together with national health authorities, scaled up its efforts to respond to this event by setting up cholera treatment centers in affected districts and providing support in water and sanitation to prevent the spread of the disease. In March, WHO and partners conducted Somalia’s first national oral cholera vaccination campaign, and successfully reached over 450 000 vulnerable people. Due to ongoing efforts, the number of cholera cases in Somalia has declined, from 13 656 cases of acute watery diarrhoea/cholera in May 2017 to 11 228 cases in June 2017.
Somalia is also facing its worst measles outbreak in 4 years, with over 14 823 suspected cases reported in 2017 (as of 31 July), compared to 5000–10 000 cases per year since 2014. The situation is especially critical for millions of under-vaccinated, weak and hungry children who are more susceptible to contracting infectious diseases. More than 80% of those affected by the current outbreak are children under 10 year of age.
In early 2017, WHO and partners, in collaboration with national health authorities, vaccinated almost 600 000 children aged 6 months to 5 years for measles in hard-to-reach and hotspot areas across the country. Despite these efforts, the transmission of measles continues, compounded by the ongoing pre-famine situation, continued mass displacement, and undernourished children living in unhygienic conditions.
In order to contain the outbreak, a nationwide campaign is planned for November 2017 to stop transmission of the disease, targeting 4.2 million children. The campaign will also intensify efforts to strengthen routine immunization and reach unvaccinated children to boost their immunity. As shown by the response to the cholera outbreak, with the right interventions, health authorities are confident that similar success may be seen in controlling the measles outbreak.
US$ 14.4 million (a cost of US$ 3.36 per child) is required by WHO and health partners to conduct the measles vaccination campaign in November 2017, of which WHO required US$ 6.8 million. To date, no funding has been received.
Related link
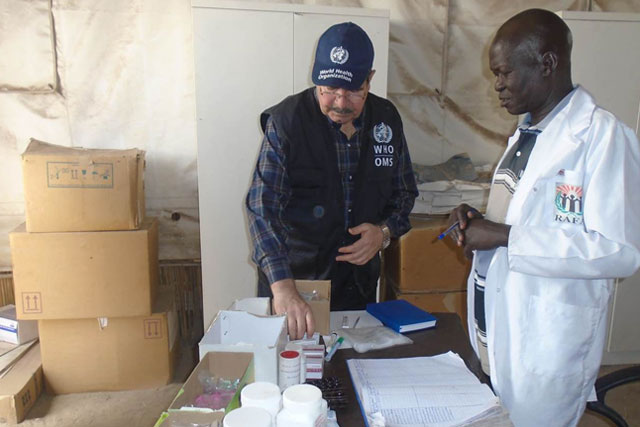
WHO responds to health needs of South Sudanese refugees in Sudan
Almost 420 000 South Sudanese refugees are currently hosted in Sudan, of whom almost 140 000 arrived in 2017. In May 2017 alone, Sudan received almost 2000 new arrivals from South Sudan every day.
The majority of refugees have settled in camps in White Nile State, while others are in East Darfur State and West/South/North Kordofan states.








 Donor alert 13 May 2019
Donor alert 13 May 2019