What is palliative care?
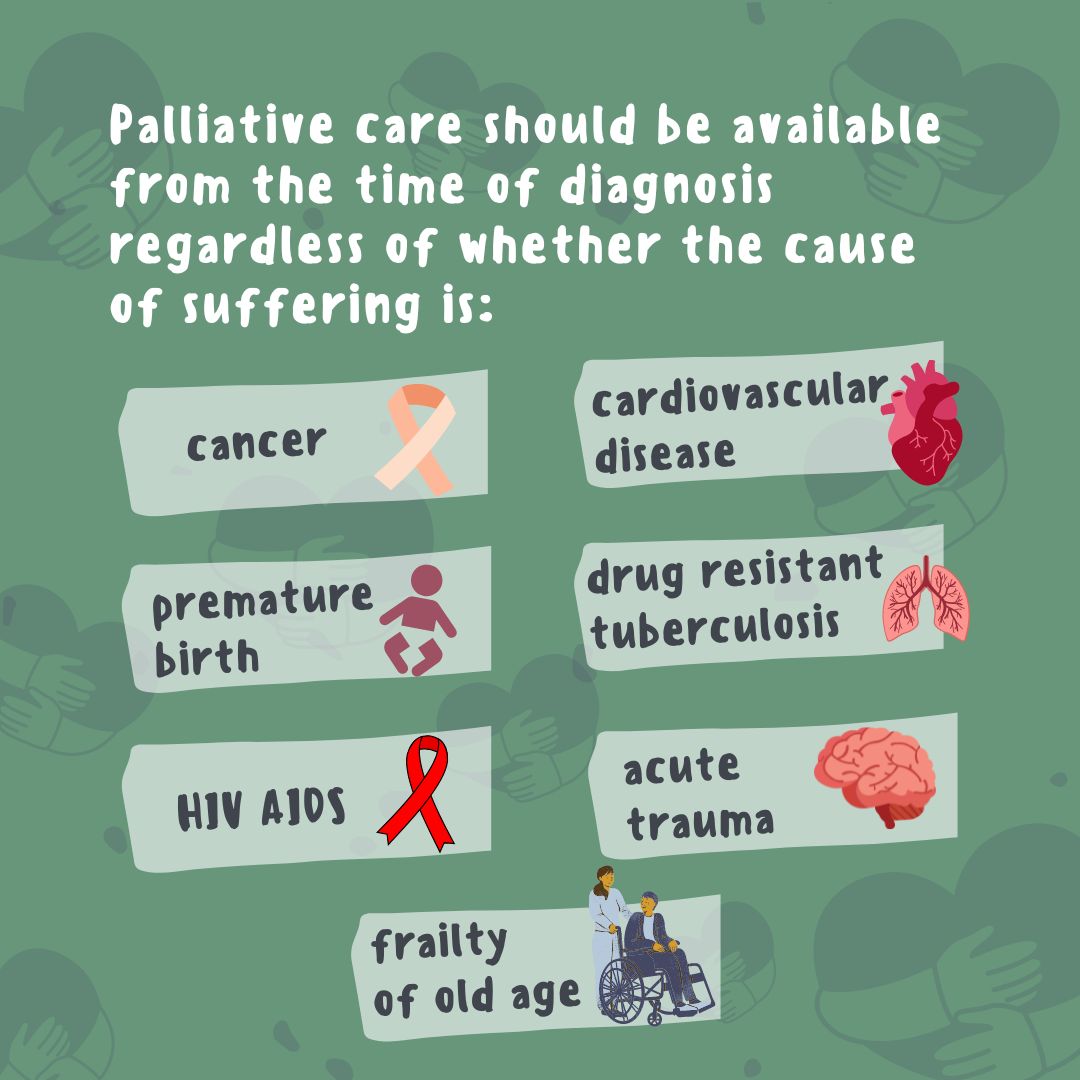
Palliative care is explicitly recognized under the human right to health and is an approach that aims to improve the quality of life of patients (adults and children) and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems—physical, psychological, social and spiritual. Palliative care is a crucial part of integrated, people-centered health services, at all levels of care and aims to relieve suffering, whether it is caused by cancer, major organ failure, drug-resistant tuberculosis, end-stage chronic illness, extreme birth prematurity or extreme frailty of old age.
When is palliative care most effective?
Palliative care is most effective when considered early in the course of the illness. Early palliative care not only improves quality of life for patients but is also a cost-saving public health intervention that reduces unnecessary hospitalizations and use of health-care services.
Palliative care at global level
At global level, the World Health Assembly Resolution 67.19 on Strengthening of palliative care as a component of comprehensive care throughout the life course, adopted in 2014, called upon WHO and Member States to improve access to palliative care as a core component of health systems, with an emphasis on primary health care and community/home-based care. Furthermore, WHO explicitly recognizes that palliative care is part of the comprehensive services required for noncommunicable diseases (NCDs) through the Global Action Plan for the Prevention and Control of NCDs 2013–2020, and fundamental to improving the quality of life, wellbeing, comfort, and human dignity for individuals, as an effective person-centered health service. Additionally, palliative care is encompassed in the definition of universal health coverage and the WHO global strategy on people-centered and integrated health services which offers a framework for strengthening palliative care programmes across diseases.
Palliative care at regional level
 At regional level, improved access to essential palliative care services is one of the regional strategic health care interventions included in the Framework for action on cancer prevention and control in the Eastern Mediterranean Region.
At regional level, improved access to essential palliative care services is one of the regional strategic health care interventions included in the Framework for action on cancer prevention and control in the Eastern Mediterranean Region.
Every year an estimated 40 million people are in need of palliative care, 78% of whom live in low- and middle-income countries. Access to palliative care services is a major challenge in the Eastern Mediterranean Region, where only an estimated 5% of adults who are in need of palliative care actually receive it. A number of significant barriers explain these unmet needs for palliative care.
National health policies and systems do not often include palliative care at all.
Training on palliative care for health professionals is often limited or non-existent.
Lack of awareness among policy-makers, health professionals and the public about what palliative care is, and the benefits it can offer patients and health systems.
Misconceptions about palliative care, such as that it is only for patients with cancer, or for the last weeks of life.
Cultural and social barriers, such as beliefs about death and dying.
Population access to opioid pain relief is inadequate and fails to meet international conventions on access to essential medicines.
Misconceptions that improving access to opioid analgesia will lead to increased substance abuse.
Palliative care in most of the Eastern Mediterranean Region remains at an early stage of development, with insufficient strategic planning by governments for palliative care services. The situation is further compounded by complicated political situations and weak health care systems coupled with conflicts affecting some countries in the Region, weakening health services and further increasing the demand for palliative care services.
Eastern Mediterranean Region Expert Network on Palliative Care
The Eastern Mediterranean Region Expert Network on Palliative Care was established in 2019 to push forward palliative care in the Region—which is becoming increasingly important given the ongoing COVID-19 pandemic and the strain it has put on health systems. The Network comprises regional and international experts, and is divided into sub-groups to deliver on different areas of work. At present, the Network has developed a road map for palliative care in the Eastern Mediterranean Region in line with the WHO Model of Palliative Care and other global guidance. The road map aims to address current gaps and inform health policy in regard to palliative care in countries of this region. It defines strategic objectives in the areas of policy, human resources and service delivery. The Network is also working on a series of policy briefs, training curricula for health care professionals, case studies showcasing models of care, and a set of indicators to monitor regional progress.
Regional webinars
Videos
Social tiles
A palliative care provider can help advocate for palliative care interventions where they are not yet accessible
Arabic
Early palliative care can improve patients’ quality of life and minimize unnecessary hospitalization
Arabic
Animated GIFs
Related links
Atlas of palliative care in the Eastern Mediterranean Region 2017
Barriers to, and opportunities for, palliative care development in the Eastern Mediterranean Region
Brief manual on health indicators monitoring global palliative care development
Framework for action on cancer prevention and control in the Eastern Mediterranean Region
Global atlas of palliative care, 2nd edition 2020
Planning and implementing palliative care services: A guide for programme managers
Why palliative care is an essential function of primary health care
What is palliative care?
Palliative care is explicitly recognized under the human right to health and is an approach that aims to improve the quality of life of patients (adults and children) and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems—physical, psychological, social and spiritual. Palliative care is a crucial part of integrated, people-centered health services, at all levels of care and aims to relieve suffering, whether it is caused by cancer, major organ failure, drug-resistant tuberculosis, end-stage chronic illness, extreme birth prematurity or extreme frailty of old age.
When is palliative care most effective?
Palliative care is most effective when considered early in the course of the illness. Early palliative care not only improves quality of life for patients but is also a cost-saving public health intervention that reduces unnecessary hospitalizations and use of health-care services.
Palliative care at global level
At global level, the World Health Assembly Resolution 67.19 on Strengthening of palliative care as a component of comprehensive care throughout the life course, adopted in 2014, called upon WHO and Member States to improve access to palliative care as a core component of health systems, with an emphasis on primary health care and community/home-based care. Furthermore, WHO explicitly recognizes that palliative care is part of the comprehensive services required for noncommunicable diseases (NCDs) through the Global Action Plan for the Prevention and Control of NCDs 2013–2020, and fundamental to improving the quality of life, wellbeing, comfort, and human dignity for individuals, as an effective person-centered health service. Additionally, palliative care is encompassed in the definition of universal health coverage and the WHO global strategy on people-centered and integrated health services which offers a framework for strengthening palliative care programmes across diseases.
Palliative care at regional level
 At regional level, improved access to essential palliative care services is one of the regional strategic health care interventions included in the Framework for action on cancer prevention and control in the Eastern Mediterranean Region.
At regional level, improved access to essential palliative care services is one of the regional strategic health care interventions included in the Framework for action on cancer prevention and control in the Eastern Mediterranean Region.
Every year an estimated 40 million people are in need of palliative care, 78% of whom live in low- and middle-income countries. Access to palliative care services is a major challenge in the Eastern Mediterranean Region, where only an estimated 5% of adults who are in need of palliative care actually receive it. A number of significant barriers explain these unmet needs for palliative care.
National health policies and systems do not often include palliative care at all.
Training on palliative care for health professionals is often limited or non-existent.
Lack of awareness among policy-makers, health professionals and the public about what palliative care is, and the benefits it can offer patients and health systems.
Misconceptions about palliative care, such as that it is only for patients with cancer, or for the last weeks of life.
Cultural and social barriers, such as beliefs about death and dying.
Population access to opioid pain relief is inadequate and fails to meet international conventions on access to essential medicines.
Misconceptions that improving access to opioid analgesia will lead to increased substance abuse.
Palliative care in most of the Eastern Mediterranean Region remains at an early stage of development, with insufficient strategic planning by governments for palliative care services. The situation is further compounded by complicated political situations and weak health care systems coupled with conflicts affecting some countries in the Region, weakening health services and further increasing the demand for palliative care services.
Eastern Mediterranean Region Expert Network on Palliative Care
The Eastern Mediterranean Region Expert Network on Palliative Care was established in 2019 to push forward palliative care in the Region—which is becoming increasingly important given the ongoing COVID-19 pandemic and the strain it has put on health systems. The Network comprises regional and international experts, and is divided into sub-groups to deliver on different areas of work. At present, the Network has developed a road map for palliative care in the Eastern Mediterranean Region in line with the WHO Model of Palliative Care and other global guidance. The road map aims to address current gaps and inform health policy in regard to palliative care in countries of this region. It defines strategic objectives in the areas of policy, human resources and service delivery. The Network is also working on a series of policy briefs, training curricula for health care professionals, case studies showcasing models of care, and a set of indicators to monitor regional progress.
Regional webinars
Videos
Social tiles
A palliative care provider can help advocate for palliative care interventions where they are not yet accessible
Arabic
Early palliative care can improve patients’ quality of life and minimize unnecessary hospitalization
Arabic
Animated GIFs
Related links
Assessing palliative care in the Eastern Mediterranean Region 2021
Atlas of palliative care in the Eastern Mediterranean Region 2017
Barriers to, and opportunities for, palliative care development in the Eastern Mediterranean Region
Brief manual on health indicators monitoring global palliative care development
Framework for action on cancer prevention and control in the Eastern Mediterranean Region
Global atlas of palliative care, 2nd edition 2020
Planning and implementing palliative care services: A guide for programme managers
Why palliative care is an essential function of primary health care