28 May 2021 – The helplessness of being called to the scene too late for patients who were previously on their way to recovery from illness or surgery, drove Dr Amal Saif Al-Maani and her colleagues to lead the race against antimicrobial resistance (AMR) upstream. Since 2015 and for more than 10 years now, they advocated for, developed and implemented a national strategy to control antimicrobial resistance.
“As an infectious disease specialist, by the time you get involved, there is nothing much you can do for the patient,” said Dr Al-Maani, Director of the Central Department for Infection Prevention and Control at the Ministry of Health in Oman.
“We need to do something earlier, to address AMR on a multisectoral level and in a more comprehensive way to tackle all aspects of the problem. At the national level, yes, but it wouldn’t work without connecting internationally with all teams globally working to stop AMR,” she said.
AMR occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death.
AMR is caused by excessive and unnecessary use of antimicrobial drugs, including antibiotics, which erodes their effect on their targeted bacteria, viruses, fungi and parasites over time — and these resistant microbes are then spread more readily where water, sanitation and hygiene are inadequate, whether in clinical or everyday settings.
Back in 2016, Dr Al-Maani set out to act on 2 fronts: boosting awareness of AMR and the importance of hand hygiene in stopping AMR, and advocating for rational use of antimicrobials.
Campaigning for hand-washing and awareness-raising
She led with her colleagues at the directorate general for diseases surveillance and control one of the largest AMR campaigns in Oman, with a particular emphasis on engaging the community, and established a system for AMR surveillance at the national level (the Oman Antimicrobial Surveillance System, or OMASS) which feeds into the Global Antimicrobial Resistance Surveillance System (GLASS).
 Dr Al-Maani describing the role of infection prevention and control in combatting the spread of AMR: 2016 national high-level ministerial meeting in Oman, the launch event for the “Oman fights AMR” national campaign. Photo: Dr Al-Maani
Dr Al-Maani describing the role of infection prevention and control in combatting the spread of AMR: 2016 national high-level ministerial meeting in Oman, the launch event for the “Oman fights AMR” national campaign. Photo: Dr Al-Maani
The campaign kicked off in May 2016 with a national high-level conference at which the National Strategic Plan for Antimicrobial Resistance, the National Antimicrobial Guidelines and National Policy for Surveillance of Multidrug Resistant Organisms were signed and launched. For 2 months, her team oversaw activities and exhibitions for community, academic institutions, agriculture and fishery sector and other sectors, private and government, in all provinces in Oman.
As part of the campaign, a role-model project on hand hygiene presented the country’s political leaders publicly advocating for hand hygiene as a main strategy to prevent transmission of infection. In parallel, hospitals CEOs, leadership and nursing administration communicated about hand hygiene to all personnel and established plans in support.
 Dr Al-Maani engaged in the national project “Be Role Model for Hand Hygiene” as part of her continuous advocacy work for hand hygiene in the community and health care settings. Photo: Dr Al-Maani
Dr Al-Maani engaged in the national project “Be Role Model for Hand Hygiene” as part of her continuous advocacy work for hand hygiene in the community and health care settings. Photo: Dr Al-Maani
The national hand hygiene project, which won Dr Al-Maani’s department the national Gold award on the World Patient Safety Day 2020, began in tertiary hospitals, after which her team took it into secondary hospitals and primary care in outpatient clinics. The effort to engage the community in infection prevention included activities in schools and for pilgrims to Mecca. Engaging students had also the positive side effect of reducing diarrhoeal diseases and respiratory infections, especially during the influenza season.
“People don’t think of AMR and their role in AMR prevention until they themselves or their loved ones become patients. In contrast, infection control professionals act much earlier,” Dr Al-Maani said.
Nipping AMR in the bud: tackling antimicrobial overuse
OMASS brings together data from the nation’s laboratory, pharmaceutical sector, and electronic medical records. It allows the health care system to target antibiotic overuse, which has immediate and longer term health costs. Having an ongoing surveillance system helps chart progress and interventions’ effectiveness.
Through this system, for instance, the team observed big increases in the use of powerful antibiotics in certain hospitals. The rise was due to certain physicians’ belief they had to cover patients whose diagnoses were still pending, before opting for a less-powerful antibiotic if and when the problem was eventually identified.
But delays or difficulties in diagnosis meant that patients were stuck on stronger antibiotics for longer, with nobody brave enough to cut the antibiotics partly for fear of potential legal repercussions, creating an environment for the growth of more resistant pathogens.
For this reason, Dr Al-Maani believes that to combat AMR, far better diagnostic tools are needed, together with new preventive and treatment methods, processes and practices that overcome the human factor in infection prevention and control.
Key to ending AMR: better, faster diagnoses and empowered health personnel
“With my background as a clinician, and a prescriber at times, I now it's challenging to decide whether or not to give a patient antibiotics when you don’t have a tool to say whether he needs it or not. We should empower the end users - the clinicians and the nurses, with better diagnostic tools to know what each patient has very early, very rapidly,” she said.
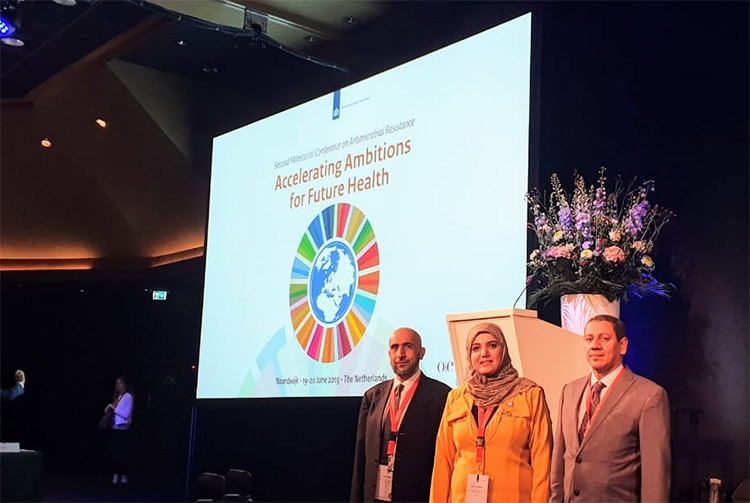 Dr Al-Maani as a member of the Oman delegation, headed by H.E. Dr. Ahmed bin Mohammed Al-Saidi, Minister of Health, at the second Ministerial Conference on Antimicrobial Resistance (AMR) hosted by the Netherlands (19-20 June 2019 in Noordwijk). Photo: Dr Al-Maani
Dr Al-Maani as a member of the Oman delegation, headed by H.E. Dr. Ahmed bin Mohammed Al-Saidi, Minister of Health, at the second Ministerial Conference on Antimicrobial Resistance (AMR) hosted by the Netherlands (19-20 June 2019 in Noordwijk). Photo: Dr Al-Maani
The pandemic brings new urgency to the AMR issue, but puts things into perspective
“If not tackled, AMR may cost the world a lot more than the pandemic has so far. COVID-19 worsens the AMR problem in 2 ways. Firstly, the unprecedented flow of patients into hospitals makes hygiene practices much more challenging, especially in full protective gear. Secondly, most clinical protocols would see COVID-19 patients given broad-spectrum antibiotics in case their fever is caused by a secondary bacterial infection. As a result, we start seeing outbreaks of resistance in pathogens in COVID-19 units around the world,” she said.
“Globally, the worry is that COVID-19 might have accelerated the spread of AMR and development of new resistant pathogens,” she states.
The response to COVID-19 has, however, also given her a renewed conviction in the world’s capability to counter AMR — but valuing preventive action.
“We all invested in the pandemic response in big ways, very fast. That has never happened before. I think it's not difficult if the world comes together and invests in ending AMR,” she said.
“I don’t exaggerate when I say that prevention is the fundamental block in the safety of any health care system. I take this opportunity to call for prioritizing the investment and innovation in the infection prevention tools so we can minimize human factors impact and prevent future health crises,” Dr Al-Maani said in her speech at the World Healthy Assembly upon accepting her award.
She also calls on WHO to put AMR at the top of its priorities as an essential step towards achieving the Sustainable Development Goals and preventing the worst health disaster of a growing pandemic.
“Let’s work for empowering infection control globally, mandating training and certification of all health care workers in infection prevention and control, investment in the innovation of more accessible, usable, convenient protective and monitoring tools, and accelerating research and development for vaccines, diagnostics and treatment.”
“The bugs are smart and keep on changing to survive so let's be more prepared and ready with new advance tools to counteract them,” she said.


