PDF version
A.F. Al-Huwaizi1 and T. Ali Rasheed2
تقييم الاحتياجات للمعالجة التقويمية للأسنان لدى المراهقين العراقيين الأكراد باستخدام منسب التجميل السني
أكرم فيصل الحويزي، تارة علي رشيد
الخلاصـة: هدف هذا المسح الذي تناول صحة الفم التعرف على الاحتياجات للمعالجة التقويمية للأسنان لدى المراهقين في السليمانية، في العراق. وقد أجرى الباحثون فحصاً سريرياً لعينة عشوائية تضم 998 من أطفال المدارس الكردية، الذين يبلغون 13 عاماً من العمر؛ وقد وجدوا أن أحراز (درجات قياس) منسب التجميل السني تتراوح بين 13 و65 ويبلغ الوسطي لها 25.4 (بانحراف معياري مقداره 9.2). وانطلاقاً من هذه الأحراز قيَّم الباحثون الاحتياجات للمعالجة على الوجه التالي: لا توجد احتياجات أو احتياجات طفيفة %58.6، احتياجات انتقائية %18.5، احتياجات مرغوبة بشدة %12.5، احتياجات إجبارية (سوء الإطباق المسبب للإعاقة) %10.3. وقد وجد الباحثون الاحتياجات للمعالجات المرغوبة بشدة أو الإجبارية (منسب التجميل السني يساوي أو يزيد على 31) في نسب مئوية متساوية لدى الذكور (%23.2) والإناث (%22.6)، ولكنها لدى سكان الأرياف (%25.1) أكثر منها لدى سكان المدن (%20.6).
ABSTRACT This oral health survey aimed to determine the orthodontic treatment needs of teenagers in Sulaimaniya, Iraq. A clinical examination was made of a random sample of 998 Kurdish schoolchildren aged 13 years. Dental Aesthetic Index (DAI) scores ranged from 13 to 65, with a mean of 25.4 (SD 9.2). From these scores, treatment needs were assessed as: no or slight need 58.6%, elective 18.5%, highly desirable 12.5% and mandatory (handicapping malocclusion) 10.3%. Highly desirable or mandatory treatment need (DAI ≥ 31) was found in equal proportions of males (23.2%) and females (22.6%), but in more rural (25.1%) than urban (20.6%) residents.
Évaluation des besoins en soins orthodontiques des adolescents kurdes iraquiens à l’aide de l’indice esthétique dentaire
RÉSUMÉ Cette enquête sur la santé bucco-dentaire visait à déterminer les besoins en soins orthodontiques des adolescents de Sulaimaniya (Iraq). Un examen clinique a été réalisé sur un échantillon aléatoire de 998 écoliers kurdes âgés de 13 ans. Les scores de l’indice esthétique dentaire (IED) étaient compris entre 13 et 65, avec une moyenne de 25,4 (écart type : 9,2). D’après ces scores, la nécessité des soins a été évaluée comme suit : pas ou peu nécessaires, 58,6 % ; facultatifs, 18,5 % ; fortement recommandés, 12,5 % ; et obligatoires (malocclusion handicapante), 10,3 %. Les niveaux de nécessité de soins « fortement recommandés » ou « obligatoires » (IED ≥ 31) se retrouvaient en proportions égales chez les garçons (23,2 %) et chez les filles (22,6 %), mais davantage chez les adolescents vivant en milieu rural (25,1 %) qu’en milieu urbain (20,6 %).
1Department of Orthodontics, College of Dentistry, University of Baghdad, Baghdad, Iraq (Correspondence to A.F. Al-Huwaizi: This email address is being protected from spambots. You need JavaScript enabled to view it.).
2Department of Orthodontics, College of Dentistry, University of Sulaimaniya, Sulaimaniya, Iraq.
Received: 22/03/07; accepted: 07/08/07
EMHJ, 2009, 15(6):1535-1541
Introduction
Many people undergo orthodontic treatment to improve their dental appearance [1]. In relation to facial aesthetics it has been shown that, from the patient’s point of view, teeth are second in importance only to background facial appearance [2]. Most individuals who have had orthodontic treatment feel that they have benefited, even though dramatic changes in facial appearance are not always evident [3].
During the 1970s, the importance of psychological factors in the assessment of malocclusion was acknowledged in the United States of America (USA) and internationally [4]. In response to the demand for an orthodontic index that includes psychosocial criteria in assessing need for orthodontic care and for use in epidemiological surveys, Cons et al. developed the Dental Aesthetic Index (DAI) using the opinions of the lay public as to what constituted unacceptable dental arrangements from an aesthetic viewpoint. It links the clinical and aesthetic components mathematically to produce a single score that combines the physical and the aesthetic aspects of occlusion [5]. The DAI has decision points along the DAI scale defining case severity levels that approximate to the judgement of orthodontists [6].
The DAI can be useful in both epidemiological surveys and as a screening device to prioritize subsidized orthodontic treatment in public programmes where resources are insufficient to meet the demand [5]. The DAI is currently being employed by the World Health Organization (WHO) as an epidemiological tool to assess unmet need for orthodontic care in its International Collaborative Study of Oral Health Outcomes [7].
Although the DAI was based on perceptions of dental aesthetics in the USA, perceptions in students in 11 diverse groups were similar to those of American students. Therefore the standard DAI can be used internationally without modification [8–11]. Because people of Kurdish ethnicity are spread across Turkey, Iraq, the Islamic Republic of Iran, Armenia and the Syrian Arab Republic very few epidemiological studies have been carried out on them. Therefore, there is no baseline data for orthodontic treatment need.
This study aimed to assess the orthodontic treatment need of Kurdish schoolchildren according to the DAI and relate it to sex and geographic location, providing baseline data that can be used in planning orthodontic treatment services.
Methods
Sample
The sample was 998 13-year-old students from 20 intermediate schools in Sulaimaniya and surrounding villages, selected according to a multi-stage stratified sampling technique described in detail in an earlier report [12]. Half the students were living in urban areas and the rest in rural areas.
Data collection
Informed consent forms were signed by the students’ parents and approval from the Ministry of Education and the school heads were obtained. The study was carried out from the beginning of October 2005 to the end of December 2005.
Each child was given a dental examination by orthodontists to determine the DAI score. The 10 DAI components are: missing visible mandibular and maxillary incisor, canine and premolar teeth (number of teeth); crowding in the incisal segment (number of crowded segments 0, 1 or 2); spacing in the incisal segment (number of spaced segments 0, 1 or 2); maxillary diastema (mm); largest maxillary anterior irregularity (mm); largest mandibular anterior irregularity (mm); anterior maxillary overjet (mm); anterior mandibular overjet (mm); vertical anterior open bite (mm); and antero-posterior molar relation (0 = normal, 1 = half cusp, 2 = full cusp). Total DAI scores are classified according to decision points that approximate to the judgement of orthodontists about treatment need: 13–25 (normal or minor malocclusion; no treatment need or slight need); 26–30 (definite malocclusion; treatment elective); 31–35 (severe malocclusion; treatment highly desirable); 36+ (very severe, handicapping malocclusion; treatment mandatory) [5].
Inter-and intra-examiner calibration were performed before the study, to ensure the consistent application of the diagnostic criteria. The results showed no statistically significant difference.
Statistical analysis
Data entry and analysis was carried out using SPSS, version 14. Student t-test was used to examine the differences of mean and standard deviation (SD) DAI scores between males and females and between urban and rural residents. P-values < 0.05 were considered significant.
Results
The total number of students examined was 1020, however 22 case sheets were excluded because of incomplete or inaccurate information, incorrect age or currently undergoing orthodontic treatment, giving a valid sample of 998: 497 males (249 urban and 248 rural) and 501 females (251 urban and 250 rural).
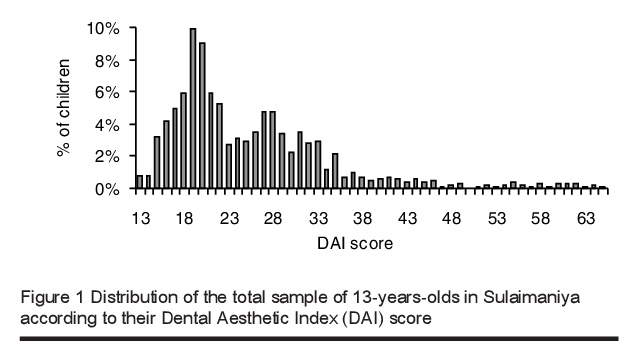
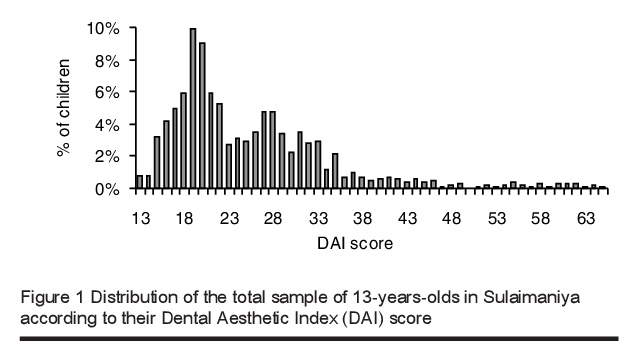
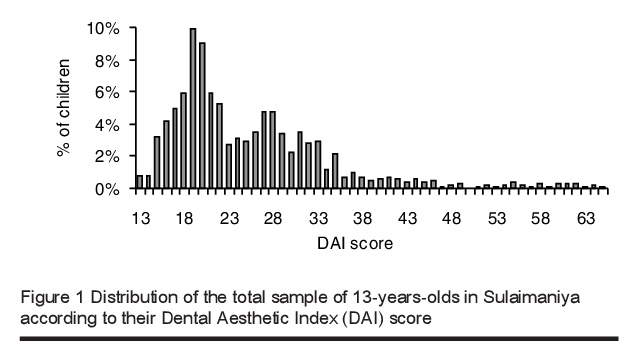
The distribution of the DAI scores for the total sample is displayed in Table 1 and Figure 1. The lowest DAI score registered in this study was 13 and the highest was 65. The most commonly registered DAI score was 19 (9.9%) followed by 20 (9.0%).
According to the DAI cut-offs, normal or minor malocclusion with no or slight treatment need (DAI 13–25) was found in 58.6% of the sample, definite malocclusion with treatment elective (DAI 26–30) in 18.5%, severe malocclusion with treatment highly desirable (DAI 31–35) in 12.5% and very severe (handicapping) malocclusion with treatment mandatory (DAI ≥ 36) in 10.3%.
DAI scores of 31+ (severe malocclusion and treatment highly desirable or mandatory) were found in similar proportions of males (23.2%) and females (22.6%), but in slightly more rural (25.1%) than urban residents (20.6%) (Table 1).
The overall mean score was 25.4 (SD 9.2). Rural males showed the highest mean DAI score [26.4 (SD 10.0) mm] followed by rural females [25.7 (SD 9.6) mm] (Table 1). There were no significant differences in mean DAI scores by sex or residence, but the mean DAI score was higher among rural residents than urban residents.
Discussion
The DAI was chosen for this research because it is simple, reliable, valid, relatively fast and accounts for both function and aesthetics. A DAI score can be obtained intraorally without the use of radiographs in about 2 minutes by trained dental auxiliaries. Previous studies found that auxiliaries were highly reliable in measuring DAI scores [5,13]. Studies in the USA as well as internationally show the validity of the DAI [8,9]. It has been adopted by the WHO, making it a universally accepted index, and it has decision points differentiating treatment priority [5,7,13–15].
To the authors' knowledge, the only published studies presenting detailed DAI score distributions are those of Jenny et al. [16], published in more detail in a later paper [14], and Al-Huwaizi [17,18]. In the present study the range of DAI scores was from 13 to 65, which is identical to that found by Al-Huwaizi in Iraq [18], whereas Cons et al. found a range of 15–66 in the USA [10].
The most commonly registered DAI scores were 19 (9.9%) and 20 (9.0%). This was comparable to the findings of Jenny et al. with 19 (9.3%) and 21 (6.6%) [14] and of Al-Huwaizi, 21 (13.1%) [18]. This result showed that the Iraqi and American samples had comparable median, lower and upper limits on the DAI scale, showing that the DAI score can be used on the Iraqi population with the same relative precision as on the American population for whom it was constructed.
According to the DAI cut-offs, treatment need was judged as no or slight in 58.6% of the sample, elective in 18.5%, highly desirable in 12.5% and mandatory in 10.3%. When comparing these results with those found by others (Table 2) our Iraqi Kurdish sample seems to have lower orthodontic treatment need than that of samples taken from American whites and natives, Australians, Japanese, New Zealanders, Spaniards, South Africans or Peruvians [6,14,16,19–25]. However, treatment need in our sample was markedly higher than that of studies done on Chinese, Australians, Nigerians, Malaysians, Iraqi Arabs and Iranians [18,19,26–30]. These differences may be attributed to differences in race, sampling techniques and environmental effects.
We found no significant sex difference in orthodontic treatment need, which agrees with some previous studies [18,22,25,31] but differs from others who found a significant difference by sex [23,24,28,30].
The prevalence of DAI scores where there was severe malocclusion and treatment was highly desirable or mandatory was higher in the rural than in the urban residents. This may be explained by the greater demand for orthodontic treatment by urban residents [32,33], who would have been excluded from the study, thus decreasing the prevalence of malocclusion in urban areas. Our result agrees with the findings of Al-Huwaizi in Iraq [18] and Esa et al. in Malaysia [28] but contradicts those of Ansai et al. in Japan [20] and Baca-Garcia et al. in Spain [22] who found that urban students had significantly higher DAI scores than rural students.
References
- Burden DJ, Pine CM. Self-perception of malocclusion among adolescents. Community dental health, 1995, 12:89–92.
- Lew KK, Foong WC, Loh E. Malocclusion prevalence in an ethnic Chinese population. Australian dental journal, 1993, 38:442–9.
- Ostler S, Kiyak HA. Treatment expectations versus outcomes among orthognathic surgery patients. International journal of adult orthodontics and orthognathic surgery, 1991, 6:247–55.
- Badwin D. Appearance and esthetics in oral health. Community dentistry and oral epidemiology, 1980, 8:244–56.
- Cons NC, Jenny J, Kohout FJ. The Dental Aesthetic Index: Iowa city [Master’s thesis]. Iowa, United States of America, University of Iowa, College of Dentistry, 1986.
- Jenny J, Cons NC. Establishing malocclusion severity levels on the Dental Aesthetic Index (DAI) scale. Australian dental journal, 1996, 41:43–6.
- International collaborative study of oral health outcomes (ICS II), document 2. Oral data collection instrument and examination criteria. Geneva, World Health Organization, 1989.
- Cons NC et al. Perceptions of occlusal conditions in Australia, the German Democratic Republic and the United States of America. International dental journal, 1983, 33:200–6.
- Cons NC et al. Utility of the Dental Aesthetic Index in industrialized and developing countries. Journal of public health dentistry, 1989, 49:163–6.
- Cons NC et al. Comparing ethnic group-specific DAI equations with the standard DAI. International dental journal, 1994, 44:153–8.
- Cons NC, Jenny J. Comparing perceptions of dental aesthetics in the USA with those in eleven ethnic groups. International dental journal, 1994, 44(5):489–94.
- Al-Huwaizi AF, Rasheed TA. Malocclusion in 13 year old Kurdish Sulaimania students. Part I: prevalence of intra-arch occlusal features. Iraqi orthodontic journal, 2006, 2(2):7–13.
- Spencer AJ, Allister JH, Brennan DS. Utility of the Dental Aesthetic Index as an orthodontic screening tool in Australia [Masters thesis]. Adelaide, Australia, University of Adelaide, 1992.
- Jenny J et al. Predicting handicapping malocclusion using the Dental Aesthetics Index (DAI). International dental journal, 1993, 43:128–32.
- Otuyemi OD, Noar JH. Variability in recording and grading the need for orthodontic treatment using the handicapping malocclusion assessment record, occlusal index and dental aesthetic index. Community dentistry and oral epidemiology, 1996, 24:222–4.
- Jenny J et al. Differences in need for orthodontic treatment between native Americans and the general population based on DAI scores. Journal of public health dentistry, 1991, 51:234–8.
- Al-Huwaizi AF. Occlusal features, perception of occlusion, orthodontic treatment need and demand among 13 year old Iraqi students (A national cross–sectional epidemiological study) [PhD thesis]. Baghdad, Iraq, University of Baghdad, 2002.
- Al-Huwaizi AF. Orthodontic treatment need (DAI) in Iraq. Iraqi orthodontic journal, 2005, 1(1):6–13.
- Spencer AJ, Allister JH, Brennan DS. Utility of the dental aesthetic index as an orthodontic screening tool in Australia, Adelaide [Masters thesis]. Adelaide, Australia, University of Adelaide, 1992.
- Ansai T et al. Prevalence of malocclusion in high school students in Japan according to the Dental Aesthetic Index. Community dentistry and oral epidemiology, 1993, 21:303–5.
- Johnson M, Harkness M. Prevalence of malocclusion and orthodontic treatment need in 10-year-old New Zealand children. Australian orthodontic journal, 2000, 16:1–8.
- Baca-Garcia A et al. Malocclusions and orthodontic treatment needs in a group of Spanish adolescents using the Dental Aesthetic Index. International dental journal, 2004, 54:138–42.
- Van Wyk PJ, Drummond RJ. Orthodontic status and treatment need of 12-year-old children in South Africa using the Dental Aesthetic Index. Journal of the South African Dental Association, 2005, 60:334–6, 338.
- Foster Page LA, Thomson WM. Malocclusion and uptake of orthodontic treatment in Taranaki 12–13-year-olds. New Zealand dental journal, 2006, 102:15.
- Bernabe E, Flores-Mir C. Orthodontic treatment need in Peruvian young adults evaluated through dental aesthetic index. Angle orthodontist, 2006, 76:417–21.
- Katoh Y et al. A comparison of DAI scores and characteristics of occlusal traits in three ethnic groups of Asian origin. International dental journal, 1998, 48(4):405–11.
- Otuyemi O et al. Malocclusion and orthodontic treatment need of secondary school students in Nigeria according to the dental aesthetic index (DAI). International dental journal, 1999, 49:203–10.
- Esa R, Razak IA, Allister JH. Epidemiology of malocclusion and orthodontic treatment need of 12–13-year-old Malaysian schoolchildren. Community dental health, 2001, 18:31–6.
- Abdullah MS, Rock WP. Assessment of orthodontic treatment need in 5,112 Malaysian children using the IOTN and DAI indices. Community dental health, 2001, 18(4):242–8.
- Danaei SM, Amirrad F, Salehi P. Orthodontic treatment needs of 12–15-year-old students in Shiraz, Islamic Republic of Iran. Eastern Mediterranean health journal, 2007, 13(2):326–34.
- Chestnutt IG et al. The orthodontic condition of children in the United Kingdom, 2003. British dental journal, 2006, 200:609–12.
- Abu Alhaija ESJ, Al-Nimri KS, Al-Khateeb SN. Self-perception of malocclusion among north Jordanian school children. European journal of orthodontics, 2005, 27:292–5.
- Al-Huwaizi AF, Al-Alousi WS, Al-Mulla AA. A national survey on perception of malocclusion among Iraq 13 year olds. Journal of the College of Dentistry, Baghdad, 2002, 14:7–16.
PDF version
A.F. Al-Huwaizi1 and T. Ali Rasheed2
تقييم الاحتياجات للمعالجة التقويمية للأسنان لدى المراهقين العراقيين الأكراد باستخدام منسب التجميل السني
أكرم فيصل الحويزي، تارة علي رشيد
الخلاصـة: هدف هذا المسح الذي تناول صحة الفم التعرف على الاحتياجات للمعالجة التقويمية للأسنان لدى المراهقين في السليمانية، في العراق. وقد أجرى الباحثون فحصاً سريرياً لعينة عشوائية تضم 998 من أطفال المدارس الكردية، الذين يبلغون 13 عاماً من العمر؛ وقد وجدوا أن أحراز (درجات قياس) منسب التجميل السني تتراوح بين 13 و65 ويبلغ الوسطي لها 25.4 (بانحراف معياري مقداره 9.2). وانطلاقاً من هذه الأحراز قيَّم الباحثون الاحتياجات للمعالجة على الوجه التالي: لا توجد احتياجات أو احتياجات طفيفة %58.6، احتياجات انتقائية %18.5، احتياجات مرغوبة بشدة %12.5، احتياجات إجبارية (سوء الإطباق المسبب للإعاقة) %10.3. وقد وجد الباحثون الاحتياجات للمعالجات المرغوبة بشدة أو الإجبارية (منسب التجميل السني يساوي أو يزيد على 31) في نسب مئوية متساوية لدى الذكور (%23.2) والإناث (%22.6)، ولكنها لدى سكان الأرياف (%25.1) أكثر منها لدى سكان المدن (%20.6).
ABSTRACT This oral health survey aimed to determine the orthodontic treatment needs of teenagers in Sulaimaniya, Iraq. A clinical examination was made of a random sample of 998 Kurdish schoolchildren aged 13 years. Dental Aesthetic Index (DAI) scores ranged from 13 to 65, with a mean of 25.4 (SD 9.2). From these scores, treatment needs were assessed as: no or slight need 58.6%, elective 18.5%, highly desirable 12.5% and mandatory (handicapping malocclusion) 10.3%. Highly desirable or mandatory treatment need (DAI ≥ 31) was found in equal proportions of males (23.2%) and females (22.6%), but in more rural (25.1%) than urban (20.6%) residents.
Évaluation des besoins en soins orthodontiques des adolescents kurdes iraquiens à l’aide de l’indice esthétique dentaire
RÉSUMÉ Cette enquête sur la santé bucco-dentaire visait à déterminer les besoins en soins orthodontiques des adolescents de Sulaimaniya (Iraq). Un examen clinique a été réalisé sur un échantillon aléatoire de 998 écoliers kurdes âgés de 13 ans. Les scores de l’indice esthétique dentaire (IED) étaient compris entre 13 et 65, avec une moyenne de 25,4 (écart type : 9,2). D’après ces scores, la nécessité des soins a été évaluée comme suit : pas ou peu nécessaires, 58,6 % ; facultatifs, 18,5 % ; fortement recommandés, 12,5 % ; et obligatoires (malocclusion handicapante), 10,3 %. Les niveaux de nécessité de soins « fortement recommandés » ou « obligatoires » (IED ≥ 31) se retrouvaient en proportions égales chez les garçons (23,2 %) et chez les filles (22,6 %), mais davantage chez les adolescents vivant en milieu rural (25,1 %) qu’en milieu urbain (20,6 %).
1Department of Orthodontics, College of Dentistry, University of Baghdad, Baghdad, Iraq (Correspondence to A.F. Al-Huwaizi: This email address is being protected from spambots. You need JavaScript enabled to view it.).
2Department of Orthodontics, College of Dentistry, University of Sulaimaniya, Sulaimaniya, Iraq.
Received: 22/03/07; accepted: 07/08/07
EMHJ, 2009, 15(6):1535-1541
Introduction
Many people undergo orthodontic treatment to improve their dental appearance [1]. In relation to facial aesthetics it has been shown that, from the patient’s point of view, teeth are second in importance only to background facial appearance [2]. Most individuals who have had orthodontic treatment feel that they have benefited, even though dramatic changes in facial appearance are not always evident [3].
During the 1970s, the importance of psychological factors in the assessment of malocclusion was acknowledged in the United States of America (USA) and internationally [4]. In response to the demand for an orthodontic index that includes psychosocial criteria in assessing need for orthodontic care and for use in epidemiological surveys, Cons et al. developed the Dental Aesthetic Index (DAI) using the opinions of the lay public as to what constituted unacceptable dental arrangements from an aesthetic viewpoint. It links the clinical and aesthetic components mathematically to produce a single score that combines the physical and the aesthetic aspects of occlusion [5]. The DAI has decision points along the DAI scale defining case severity levels that approximate to the judgement of orthodontists [6].
The DAI can be useful in both epidemiological surveys and as a screening device to prioritize subsidized orthodontic treatment in public programmes where resources are insufficient to meet the demand [5]. The DAI is currently being employed by the World Health Organization (WHO) as an epidemiological tool to assess unmet need for orthodontic care in its International Collaborative Study of Oral Health Outcomes [7].
Although the DAI was based on perceptions of dental aesthetics in the USA, perceptions in students in 11 diverse groups were similar to those of American students. Therefore the standard DAI can be used internationally without modification [8–11]. Because people of Kurdish ethnicity are spread across Turkey, Iraq, the Islamic Republic of Iran, Armenia and the Syrian Arab Republic very few epidemiological studies have been carried out on them. Therefore, there is no baseline data for orthodontic treatment need.
This study aimed to assess the orthodontic treatment need of Kurdish schoolchildren according to the DAI and relate it to sex and geographic location, providing baseline data that can be used in planning orthodontic treatment services.
Methods
Sample
The sample was 998 13-year-old students from 20 intermediate schools in Sulaimaniya and surrounding villages, selected according to a multi-stage stratified sampling technique described in detail in an earlier report [12]. Half the students were living in urban areas and the rest in rural areas.
Data collection
Informed consent forms were signed by the students’ parents and approval from the Ministry of Education and the school heads were obtained. The study was carried out from the beginning of October 2005 to the end of December 2005.
Each child was given a dental examination by orthodontists to determine the DAI score. The 10 DAI components are: missing visible mandibular and maxillary incisor, canine and premolar teeth (number of teeth); crowding in the incisal segment (number of crowded segments 0, 1 or 2); spacing in the incisal segment (number of spaced segments 0, 1 or 2); maxillary diastema (mm); largest maxillary anterior irregularity (mm); largest mandibular anterior irregularity (mm); anterior maxillary overjet (mm); anterior mandibular overjet (mm); vertical anterior open bite (mm); and antero-posterior molar relation (0 = normal, 1 = half cusp, 2 = full cusp). Total DAI scores are classified according to decision points that approximate to the judgement of orthodontists about treatment need: 13–25 (normal or minor malocclusion; no treatment need or slight need); 26–30 (definite malocclusion; treatment elective); 31–35 (severe malocclusion; treatment highly desirable); 36+ (very severe, handicapping malocclusion; treatment mandatory) [5].
Inter-and intra-examiner calibration were performed before the study, to ensure the consistent application of the diagnostic criteria. The results showed no statistically significant difference.
Statistical analysis
Data entry and analysis was carried out using SPSS, version 14. Student t-test was used to examine the differences of mean and standard deviation (SD) DAI scores between males and females and between urban and rural residents. P-values < 0.05 were considered significant.
Results
The total number of students examined was 1020, however 22 case sheets were excluded because of incomplete or inaccurate information, incorrect age or currently undergoing orthodontic treatment, giving a valid sample of 998: 497 males (249 urban and 248 rural) and 501 females (251 urban and 250 rural).
The distribution of the DAI scores for the total sample is displayed in Table 1 and Figure 1. The lowest DAI score registered in this study was 13 and the highest was 65. The most commonly registered DAI score was 19 (9.9%) followed by 20 (9.0%).
According to the DAI cut-offs, normal or minor malocclusion with no or slight treatment need (DAI 13–25) was found in 58.6% of the sample, definite malocclusion with treatment elective (DAI 26–30) in 18.5%, severe malocclusion with treatment highly desirable (DAI 31–35) in 12.5% and very severe (handicapping) malocclusion with treatment mandatory (DAI ≥ 36) in 10.3%.
DAI scores of 31+ (severe malocclusion and treatment highly desirable or mandatory) were found in similar proportions of males (23.2%) and females (22.6%), but in slightly more rural (25.1%) than urban residents (20.6%) (Table 1).
The overall mean score was 25.4 (SD 9.2). Rural males showed the highest mean DAI score [26.4 (SD 10.0) mm] followed by rural females [25.7 (SD 9.6) mm] (Table 1). There were no significant differences in mean DAI scores by sex or residence, but the mean DAI score was higher among rural residents than urban residents.
Discussion
The DAI was chosen for this research because it is simple, reliable, valid, relatively fast and accounts for both function and aesthetics. A DAI score can be obtained intraorally without the use of radiographs in about 2 minutes by trained dental auxiliaries. Previous studies found that auxiliaries were highly reliable in measuring DAI scores [5,13]. Studies in the USA as well as internationally show the validity of the DAI [8,9]. It has been adopted by the WHO, making it a universally accepted index, and it has decision points differentiating treatment priority [5,7,13–15].
To the authors' knowledge, the only published studies presenting detailed DAI score distributions are those of Jenny et al. [16], published in more detail in a later paper [14], and Al-Huwaizi [17,18]. In the present study the range of DAI scores was from 13 to 65, which is identical to that found by Al-Huwaizi in Iraq [18], whereas Cons et al. found a range of 15–66 in the USA [10].
The most commonly registered DAI scores were 19 (9.9%) and 20 (9.0%). This was comparable to the findings of Jenny et al. with 19 (9.3%) and 21 (6.6%) [14] and of Al-Huwaizi, 21 (13.1%) [18]. This result showed that the Iraqi and American samples had comparable median, lower and upper limits on the DAI scale, showing that the DAI score can be used on the Iraqi population with the same relative precision as on the American population for whom it was constructed.
According to the DAI cut-offs, treatment need was judged as no or slight in 58.6% of the sample, elective in 18.5%, highly desirable in 12.5% and mandatory in 10.3%. When comparing these results with those found by others (Table 2) our Iraqi Kurdish sample seems to have lower orthodontic treatment need than that of samples taken from American whites and natives, Australians, Japanese, New Zealanders, Spaniards, South Africans or Peruvians [6,14,16,19–25]. However, treatment need in our sample was markedly higher than that of studies done on Chinese, Australians, Nigerians, Malaysians, Iraqi Arabs and Iranians [18,19,26–30]. These differences may be attributed to differences in race, sampling techniques and environmental effects.
We found no significant sex difference in orthodontic treatment need, which agrees with some previous studies [18,22,25,31] but differs from others who found a significant difference by sex [23,24,28,30].
The prevalence of DAI scores where there was severe malocclusion and treatment was highly desirable or mandatory was higher in the rural than in the urban residents. This may be explained by the greater demand for orthodontic treatment by urban residents [32,33], who would have been excluded from the study, thus decreasing the prevalence of malocclusion in urban areas. Our result agrees with the findings of Al-Huwaizi in Iraq [18] and Esa et al. in Malaysia [28] but contradicts those of Ansai et al. in Japan [20] and Baca-Garcia et al. in Spain [22] who found that urban students had significantly higher DAI scores than rural students.
References
- Burden DJ, Pine CM. Self-perception of malocclusion among adolescents. Community dental health, 1995, 12:89–92.
- Lew KK, Foong WC, Loh E. Malocclusion prevalence in an ethnic Chinese population. Australian dental journal, 1993, 38:442–9.
- Ostler S, Kiyak HA. Treatment expectations versus outcomes among orthognathic surgery patients. International journal of adult orthodontics and orthognathic surgery, 1991, 6:247–55.
- Badwin D. Appearance and esthetics in oral health. Community dentistry and oral epidemiology, 1980, 8:244–56.
- Cons NC, Jenny J, Kohout FJ. The Dental Aesthetic Index: Iowa city [Master’s thesis]. Iowa, United States of America, University of Iowa, College of Dentistry, 1986.
- Jenny J, Cons NC. Establishing malocclusion severity levels on the Dental Aesthetic Index (DAI) scale. Australian dental journal, 1996, 41:43–6.
- International collaborative study of oral health outcomes (ICS II), document 2. Oral data collection instrument and examination criteria. Geneva, World Health Organization, 1989.
- Cons NC et al. Perceptions of occlusal conditions in Australia, the German Democratic Republic and the United States of America. International dental journal, 1983, 33:200–6.
- Cons NC et al. Utility of the Dental Aesthetic Index in industrialized and developing countries. Journal of public health dentistry, 1989, 49:163–6.
- Cons NC et al. Comparing ethnic group-specific DAI equations with the standard DAI. International dental journal, 1994, 44:153–8.
- Cons NC, Jenny J. Comparing perceptions of dental aesthetics in the USA with those in eleven ethnic groups. International dental journal, 1994, 44(5):489–94.
- Al-Huwaizi AF, Rasheed TA. Malocclusion in 13 year old Kurdish Sulaimania students. Part I: prevalence of intra-arch occlusal features. Iraqi orthodontic journal, 2006, 2(2):7–13.
- Spencer AJ, Allister JH, Brennan DS. Utility of the Dental Aesthetic Index as an orthodontic screening tool in Australia [Masters thesis]. Adelaide, Australia, University of Adelaide, 1992.
- Jenny J et al. Predicting handicapping malocclusion using the Dental Aesthetics Index (DAI). International dental journal, 1993, 43:128–32.
- Otuyemi OD, Noar JH. Variability in recording and grading the need for orthodontic treatment using the handicapping malocclusion assessment record, occlusal index and dental aesthetic index. Community dentistry and oral epidemiology, 1996, 24:222–4.
- Jenny J et al. Differences in need for orthodontic treatment between native Americans and the general population based on DAI scores. Journal of public health dentistry, 1991, 51:234–8.
- Al-Huwaizi AF. Occlusal features, perception of occlusion, orthodontic treatment need and demand among 13 year old Iraqi students (A national cross–sectional epidemiological study) [PhD thesis]. Baghdad, Iraq, University of Baghdad, 2002.
- Al-Huwaizi AF. Orthodontic treatment need (DAI) in Iraq. Iraqi orthodontic journal, 2005, 1(1):6–13.
- Spencer AJ, Allister JH, Brennan DS. Utility of the dental aesthetic index as an orthodontic screening tool in Australia, Adelaide [Masters thesis]. Adelaide, Australia, University of Adelaide, 1992.
- Ansai T et al. Prevalence of malocclusion in high school students in Japan according to the Dental Aesthetic Index. Community dentistry and oral epidemiology, 1993, 21:303–5.
- Johnson M, Harkness M. Prevalence of malocclusion and orthodontic treatment need in 10-year-old New Zealand children. Australian orthodontic journal, 2000, 16:1–8.
- Baca-Garcia A et al. Malocclusions and orthodontic treatment needs in a group of Spanish adolescents using the Dental Aesthetic Index. International dental journal, 2004, 54:138–42.
- Van Wyk PJ, Drummond RJ. Orthodontic status and treatment need of 12-year-old children in South Africa using the Dental Aesthetic Index. Journal of the South African Dental Association, 2005, 60:334–6, 338.
- Foster Page LA, Thomson WM. Malocclusion and uptake of orthodontic treatment in Taranaki 12–13-year-olds. New Zealand dental journal, 2006, 102:15.
- Bernabe E, Flores-Mir C. Orthodontic treatment need in Peruvian young adults evaluated through dental aesthetic index. Angle orthodontist, 2006, 76:417–21.
- Katoh Y et al. A comparison of DAI scores and characteristics of occlusal traits in three ethnic groups of Asian origin. International dental journal, 1998, 48(4):405–11.
- Otuyemi O et al. Malocclusion and orthodontic treatment need of secondary school students in Nigeria according to the dental aesthetic index (DAI). International dental journal, 1999, 49:203–10.
- Esa R, Razak IA, Allister JH. Epidemiology of malocclusion and orthodontic treatment need of 12–13-year-old Malaysian schoolchildren. Community dental health, 2001, 18:31–6.
- Abdullah MS, Rock WP. Assessment of orthodontic treatment need in 5,112 Malaysian children using the IOTN and DAI indices. Community dental health, 2001, 18(4):242–8.
- Danaei SM, Amirrad F, Salehi P. Orthodontic treatment needs of 12–15-year-old students in Shiraz, Islamic Republic of Iran. Eastern Mediterranean health journal, 2007, 13(2):326–34.
- Chestnutt IG et al. The orthodontic condition of children in the United Kingdom, 2003. British dental journal, 2006, 200:609–12.
- Abu Alhaija ESJ, Al-Nimri KS, Al-Khateeb SN. Self-perception of malocclusion among north Jordanian school children. European journal of orthodontics, 2005, 27:292–5.
- Al-Huwaizi AF, Al-Alousi WS, Al-Mulla AA. A national survey on perception of malocclusion among Iraq 13 year olds. Journal of the College of Dentistry, Baghdad, 2002, 14:7–16.