PDF version
M.H.A. Shalchi 1 and R. Daneshvar1
1Khatam Al-Anbia Eye Hospital, Mashhad University of Medical Sciences, Mashhad, Islamic Republic of Iran (Correspondence to R. Daneshvar: This email address is being protected from spambots. You need JavaScript enabled to view it.).
Received: 21/05/07; accepted: 18/06/07
EMHJ, 2009, 15(6):1613-1616
Introduction
Retinal artery occlusion causes catastrophic, sudden visual loss. It is a true ophthalmic emergency in which every minute of delay increases the risk of irreversible retinal damage [1]. More than 90% of eyes with central retinal artery occlusion (CRAO) have a sudden, painless decrease in visual acuity to a level of counting fingers to light perception [2].
More than 150 years since the description of the characteristic features and the presumed cause of CRAO by von Graefe, this disease remains a therapeutic dilemma [3]. A variety of treatments have been proposed, but none of them show a clear therapeutic benefit or have wide acceptance [3]. Thus most physicians tend to use a combination of treatments with low potential side-effects. The most popular of these are ocular massage, rebreathing with carbogen, oral acetazolamide and topical antiglaucomatous agents. Attempts have been made to treat the disease with systemic anticoagulation/antiaggregation therapy, transluminal laser embolysis and selective intra-arterial lysis of the clot [3]. Heparin and acetylsalicylic acid are not very effective, and intra-arterial lysis is under active investigation by the European Assessment Group for Lysis in the Eye (EAGLE) trial [3].
To the best of our knowledge, there are few reports on laser-assisted transluminal embolysis, and there are only 2 reports on successful neodymium:yttrium-aluminium-garnet (Nd:YAG) laser treatment of embolic CRAO [4,5]. We report here on another successful use of Reynard and Hanscom’s method [4], with some modifications, for the treatment of retinal artery occlusion.
Case presentation
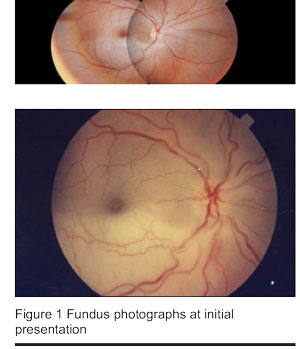
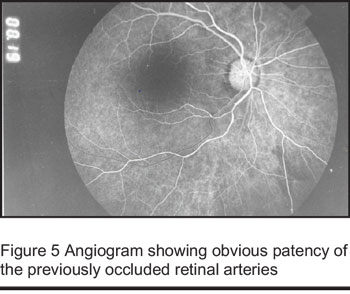
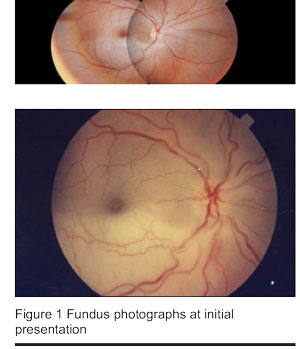
A 38-year-old woman presented to the emergency department with a 30-hour history of sudden, painless visual loss in her right eye. There was no history of cardiovascular disease or hypertension. Her ocular history was unremarkable, except for a dacryocystorhinostomy procedure performed 5 months previously. Physical examination revealed a visual acuity of 2/400 in the right eye, which was more preserved in the temporal field. There was a moderate relative afferent pupillary defect of the right eye. The ocular motilities were unlimited and there was no significant pathology in the anterior segment. The intraocular pressure was normal. On indirect binocular ophthalmoscopy, there was a somewhat oedematous optic nerve head, with an obvious cherry-red spot in the macular area (Figure 1). An embolus was visible at the bifurcation of the inferior retinal artery. The lower half of the retina was pale and oedematous, with no obvious blood flow. The left eye, with a visual acuity of 25/20, was normal in physical examination.
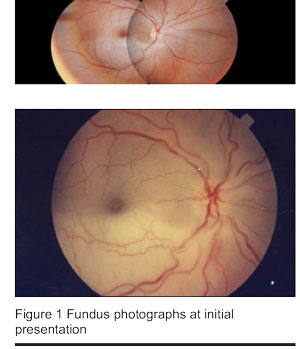
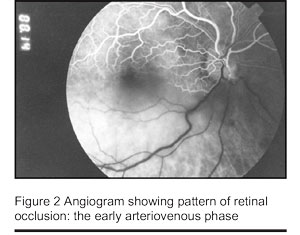
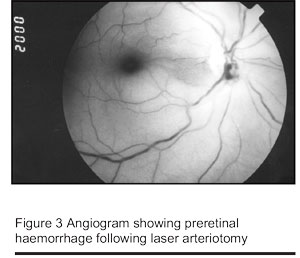
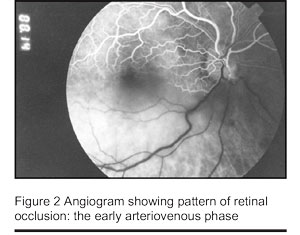
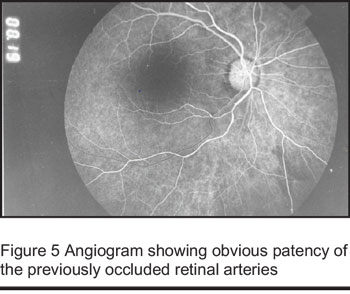
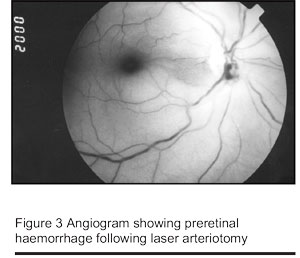
Inferior hemiretinal arterial occlusion was diagnosed. The patient was informed about the prognosis and treatment was started. On-the-spot fundus photography and fluorescein angiography confirmed the complete vascular occlusion as the main pathology (Figure 2). With the written consent of the patient, transluminal Nd:YAG laser embolysis (TYE) was attempted. The laser beam (Nd:YAG laser, 9900YAG, Coherent Medical, UK) was focused on the embolus, using a Mainster Standard fundus contact lens (Ocular, California, USA). The first shot with a power of 1 mJ was unsuccessful in dislodging the embolus. A second shot of 1.2 mJ seemed to produce some tissue reaction and minimal change in the embolus with a minute preretinal haemorrhage. Although producing more bleeding, the third and last pulse of 1.8 mJ successfully dissolved the embolus and blood flow was regained in the territory of the previously occluded vessels (Figure 3). The next phases of fluorescein angiography showed the blood flow in the affected artery. There was an immediate subjective improvement in the patient’s vision.
A cardiovascular evaluation was requested that revealed a prolapsed, thickened anterior cusp of the mitral valve with mild regurgitation, which was the possible source of the embolus.
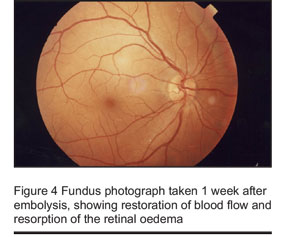
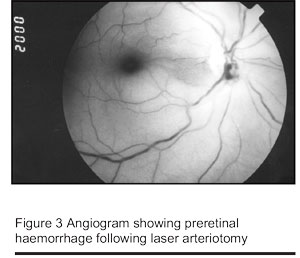
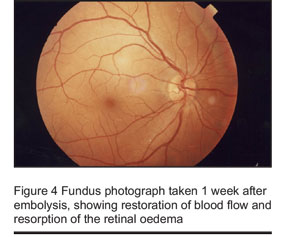
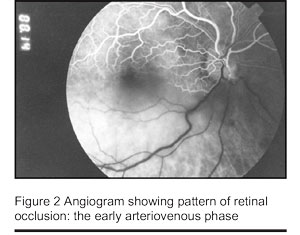
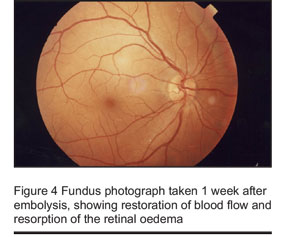
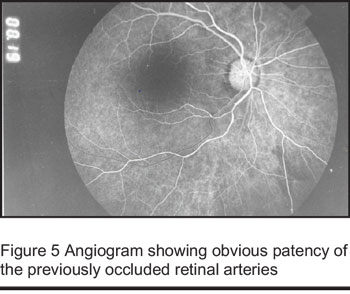
The next day, the patient’s vision improved to 15/400 and there was no change in the preretinal haemorrhage. The intraocular pressure remained within normal limits. On a follow-up visit 1 week later, the patient had a visual acuity of 25/400 and improved visual field, with resolution of the retinal oedema and normal appearing blood flow of the inferior hemiretina (Figure 4). The haemorrhage had been resorbed and the angiograms confirmed the patency of the arterial lumens in the affected vessels (Figure 5). The intraocular pressure remained normal. One month later the retinal artery was still patent but there was no further improvement in the patient’s vision. Ten months and 18 months later, the patient’s visual acuity and ophthalmic examinations were unchanged. There were no specific complications such as choroidal neovascularization.
Discussion
The patient had immediate and dramatic restoration of the patency of the occluded retinal arterioles after the TYE procedure. Fluorescein angiography confirmed these findings in the immediate post-lysis phase and during the 18 months of follow-up. Also, there were subjective and objective improvements of vision with stable, improved ophthalmic findings.
Despite the grave prognosis of CRAO, the natural history for recovery of vision after branch retinal artery occlusion (BRAO) and cilioretinal artery occlusion is actually quite favourable. Visual acuity in 80% of eyes with BRAO will eventually improve to 20/40, and the prognosis is even better for cilioretinal artery occlusion, which demonstrates a 90% and 60% rate of improvement to more than 20/40 and 20/20 visual acuity, respectively [6]. In our patient, however, the unchanging clinical course over the first 30 hours and the immediate response to treatment suggest that spontaneous resolution was unlikely to occur. Experimental data show that retinal ischaemia for 97 minutes induces no detectable damage, but after that time, the longer the CRAO, the more severe the irreversible damage [7]. The experiments of Hayreh et al. suggested that CRAO lasting for about 240 minutes results in massive irreversible retinal damage [7], which explains the poor final visual acuity in our patient.
According to Opremcak and Benner the Nd:YAG laser pulse shatters the embolus, leaving the vessel wall intact due its greater elasticity and lower absorbency of infrared irradiation [6]. In our patient photodisruption and fragmentation of the embolus resulted in immediate restoration of retinal blood flow and was associated with an immediate improvement of visual function. TYE may also lend itself to the treatment of CRAO in cases where the embolus is visible. The risks of TYE treatment—e.g. retinal and vitreous haemorrhage, retinal tears, choroidal neovascularization and epiretinal membrane formation—must be weighed against the likely permanent loss of vision due to CRAO.
Prior attempts at laser treatment for retinal artery emboli have shown different outcomes and success rates. Dutton and Craig [1] and Ciulla et al. [8] reported the failure of argon laser treatment for retinal emboli. However, Opremcak and Benner observed recovery of vision in a TYE-treated patient with BRAO and another patient with cilioretinal artery occlusion [6]. Reports of Reynard and Hanscom on the successful treatment of CRAO with TYE provide further support for this technique as a new treatment modality in patients suffering from catastrophic retinal arterial occlusion [4]. Feist and Emond reported on a dramatic response to TYE in a patient with a 1-week history of CRAO [5]. Our patient had a similar, considerable improvement in visual acuity, despite the long period of arterial occlusion.
The technique might be beneficial in eyes with CRAO where an embolus is visible. Emboli are visible in 20%–40% of eyes with CRAO and are associated with worse vision [2]. However, further investigations about the long-term efficacy and potential side-effects of laser embolysis is essential before using the treatment as a first-line therapeutic option in patients with retinal artery occlusion.
Conclusion
Transluminal Nd:YAG laser arteriotomy and embolectomy showed promising results in restoration of blood flow to the ischaemic retina in a patient with retinal arterial occlusion due to visible emboli. However, controlled clinical trials are necessary before adoption of the method as a first-line therapy for these patients.
References
- Dutton GN, Craig G. Treatment of retinal embolism by photocoagulation. British journal of ophthalmology, 1989, 73:580–1.
- Sharma S, Brown GC. Retinal artery obstruction. In: Ryan SJ, Schachat AP, eds. Retina, 3rd ed. Volume 2. St Louis, Mosby, 2001:1350–9.
- Muller AJ et al. Evaluation of minimally invasive therapies and rationale for a prospective randomized trial to evaluate selective intra-arterial lysis for clinically complete central retinal artery occlusion. Archives of ophthalmology 2003, 121(10):1377–81.
- Reynard M, Hanscom T. Neodymium: yttrium-aluminum-garnet laser arteriotomy with embolectomy for central retinal artery occlusion. American journal of ophthalmology, 2004, 137(1):196–8.
- Feist RM, Emond TL. Transluminal Nd:YAG laser embolysis for central retinal artery occlusion. Retina, 2005, 25(6):797–9.
- Opremcak EM, Benner JD. Transluminal Nd:YAG laser embolysis for branch retinal artery occlusion. Retina, 2002, 22(2):213–6.
- Hayreh SS et al. Central retinal artery occlusion. Retinal survival time. Experimental eye research, 2004, 78(3):723–36.
- Ciulla TA, D’Amico DJ, Miller JW. Laser photocoagulation of visible retinal artery emboli. British journal of ophthalmology, 1995, 79(10):964–5.
PDF version
M.H.A. Shalchi 1 and R. Daneshvar1
1Khatam Al-Anbia Eye Hospital, Mashhad University of Medical Sciences, Mashhad, Islamic Republic of Iran (Correspondence to R. Daneshvar: This email address is being protected from spambots. You need JavaScript enabled to view it.).
Received: 21/05/07; accepted: 18/06/07
EMHJ, 2009, 15(6):1613-1616
Introduction
Retinal artery occlusion causes catastrophic, sudden visual loss. It is a true ophthalmic emergency in which every minute of delay increases the risk of irreversible retinal damage [1]. More than 90% of eyes with central retinal artery occlusion (CRAO) have a sudden, painless decrease in visual acuity to a level of counting fingers to light perception [2].
More than 150 years since the description of the characteristic features and the presumed cause of CRAO by von Graefe, this disease remains a therapeutic dilemma [3]. A variety of treatments have been proposed, but none of them show a clear therapeutic benefit or have wide acceptance [3]. Thus most physicians tend to use a combination of treatments with low potential side-effects. The most popular of these are ocular massage, rebreathing with carbogen, oral acetazolamide and topical antiglaucomatous agents. Attempts have been made to treat the disease with systemic anticoagulation/antiaggregation therapy, transluminal laser embolysis and selective intra-arterial lysis of the clot [3]. Heparin and acetylsalicylic acid are not very effective, and intra-arterial lysis is under active investigation by the European Assessment Group for Lysis in the Eye (EAGLE) trial [3].
To the best of our knowledge, there are few reports on laser-assisted transluminal embolysis, and there are only 2 reports on successful neodymium:yttrium-aluminium-garnet (Nd:YAG) laser treatment of embolic CRAO [4,5]. We report here on another successful use of Reynard and Hanscom’s method [4], with some modifications, for the treatment of retinal artery occlusion.
Case presentation
A 38-year-old woman presented to the emergency department with a 30-hour history of sudden, painless visual loss in her right eye. There was no history of cardiovascular disease or hypertension. Her ocular history was unremarkable, except for a dacryocystorhinostomy procedure performed 5 months previously. Physical examination revealed a visual acuity of 2/400 in the right eye, which was more preserved in the temporal field. There was a moderate relative afferent pupillary defect of the right eye. The ocular motilities were unlimited and there was no significant pathology in the anterior segment. The intraocular pressure was normal. On indirect binocular ophthalmoscopy, there was a somewhat oedematous optic nerve head, with an obvious cherry-red spot in the macular area (Figure 1). An embolus was visible at the bifurcation of the inferior retinal artery. The lower half of the retina was pale and oedematous, with no obvious blood flow. The left eye, with a visual acuity of 25/20, was normal in physical examination.
Inferior hemiretinal arterial occlusion was diagnosed. The patient was informed about the prognosis and treatment was started. On-the-spot fundus photography and fluorescein angiography confirmed the complete vascular occlusion as the main pathology (Figure 2). With the written consent of the patient, transluminal Nd:YAG laser embolysis (TYE) was attempted. The laser beam (Nd:YAG laser, 9900YAG, Coherent Medical, UK) was focused on the embolus, using a Mainster Standard fundus contact lens (Ocular, California, USA). The first shot with a power of 1 mJ was unsuccessful in dislodging the embolus. A second shot of 1.2 mJ seemed to produce some tissue reaction and minimal change in the embolus with a minute preretinal haemorrhage. Although producing more bleeding, the third and last pulse of 1.8 mJ successfully dissolved the embolus and blood flow was regained in the territory of the previously occluded vessels (Figure 3). The next phases of fluorescein angiography showed the blood flow in the affected artery. There was an immediate subjective improvement in the patient’s vision.
A cardiovascular evaluation was requested that revealed a prolapsed, thickened anterior cusp of the mitral valve with mild regurgitation, which was the possible source of the embolus.
The next day, the patient’s vision improved to 15/400 and there was no change in the preretinal haemorrhage. The intraocular pressure remained within normal limits. On a follow-up visit 1 week later, the patient had a visual acuity of 25/400 and improved visual field, with resolution of the retinal oedema and normal appearing blood flow of the inferior hemiretina (Figure 4). The haemorrhage had been resorbed and the angiograms confirmed the patency of the arterial lumens in the affected vessels (Figure 5). The intraocular pressure remained normal. One month later the retinal artery was still patent but there was no further improvement in the patient’s vision. Ten months and 18 months later, the patient’s visual acuity and ophthalmic examinations were unchanged. There were no specific complications such as choroidal neovascularization.
Discussion
The patient had immediate and dramatic restoration of the patency of the occluded retinal arterioles after the TYE procedure. Fluorescein angiography confirmed these findings in the immediate post-lysis phase and during the 18 months of follow-up. Also, there were subjective and objective improvements of vision with stable, improved ophthalmic findings.
Despite the grave prognosis of CRAO, the natural history for recovery of vision after branch retinal artery occlusion (BRAO) and cilioretinal artery occlusion is actually quite favourable. Visual acuity in 80% of eyes with BRAO will eventually improve to 20/40, and the prognosis is even better for cilioretinal artery occlusion, which demonstrates a 90% and 60% rate of improvement to more than 20/40 and 20/20 visual acuity, respectively [6]. In our patient, however, the unchanging clinical course over the first 30 hours and the immediate response to treatment suggest that spontaneous resolution was unlikely to occur. Experimental data show that retinal ischaemia for 97 minutes induces no detectable damage, but after that time, the longer the CRAO, the more severe the irreversible damage [7]. The experiments of Hayreh et al. suggested that CRAO lasting for about 240 minutes results in massive irreversible retinal damage [7], which explains the poor final visual acuity in our patient.
According to Opremcak and Benner the Nd:YAG laser pulse shatters the embolus, leaving the vessel wall intact due its greater elasticity and lower absorbency of infrared irradiation [6]. In our patient photodisruption and fragmentation of the embolus resulted in immediate restoration of retinal blood flow and was associated with an immediate improvement of visual function. TYE may also lend itself to the treatment of CRAO in cases where the embolus is visible. The risks of TYE treatment—e.g. retinal and vitreous haemorrhage, retinal tears, choroidal neovascularization and epiretinal membrane formation—must be weighed against the likely permanent loss of vision due to CRAO.
Prior attempts at laser treatment for retinal artery emboli have shown different outcomes and success rates. Dutton and Craig [1] and Ciulla et al. [8] reported the failure of argon laser treatment for retinal emboli. However, Opremcak and Benner observed recovery of vision in a TYE-treated patient with BRAO and another patient with cilioretinal artery occlusion [6]. Reports of Reynard and Hanscom on the successful treatment of CRAO with TYE provide further support for this technique as a new treatment modality in patients suffering from catastrophic retinal arterial occlusion [4]. Feist and Emond reported on a dramatic response to TYE in a patient with a 1-week history of CRAO [5]. Our patient had a similar, considerable improvement in visual acuity, despite the long period of arterial occlusion.
The technique might be beneficial in eyes with CRAO where an embolus is visible. Emboli are visible in 20%–40% of eyes with CRAO and are associated with worse vision [2]. However, further investigations about the long-term efficacy and potential side-effects of laser embolysis is essential before using the treatment as a first-line therapeutic option in patients with retinal artery occlusion.
Conclusion
Transluminal Nd:YAG laser arteriotomy and embolectomy showed promising results in restoration of blood flow to the ischaemic retina in a patient with retinal arterial occlusion due to visible emboli. However, controlled clinical trials are necessary before adoption of the method as a first-line therapy for these patients.
References
- Dutton GN, Craig G. Treatment of retinal embolism by photocoagulation. British journal of ophthalmology, 1989, 73:580–1.
- Sharma S, Brown GC. Retinal artery obstruction. In: Ryan SJ, Schachat AP, eds. Retina, 3rd ed. Volume 2. St Louis, Mosby, 2001:1350–9.
- Muller AJ et al. Evaluation of minimally invasive therapies and rationale for a prospective randomized trial to evaluate selective intra-arterial lysis for clinically complete central retinal artery occlusion. Archives of ophthalmology 2003, 121(10):1377–81.
- Reynard M, Hanscom T. Neodymium: yttrium-aluminum-garnet laser arteriotomy with embolectomy for central retinal artery occlusion. American journal of ophthalmology, 2004, 137(1):196–8.
- Feist RM, Emond TL. Transluminal Nd:YAG laser embolysis for central retinal artery occlusion. Retina, 2005, 25(6):797–9.
- Opremcak EM, Benner JD. Transluminal Nd:YAG laser embolysis for branch retinal artery occlusion. Retina, 2002, 22(2):213–6.
- Hayreh SS et al. Central retinal artery occlusion. Retinal survival time. Experimental eye research, 2004, 78(3):723–36.
- Ciulla TA, D’Amico DJ, Miller JW. Laser photocoagulation of visible retinal artery emboli. British journal of ophthalmology, 1995, 79(10):964–5.