PDF version
N.E. Hassan,1 S.A. El-Masry1 and A.E. El-Sawaf1
محيط الخصر وتراكم الشحوم المركزي لدى الأطفال المصريـين في المدارس الابتدائية
نـيِّرة المرسي حسن، سحر عبد الرؤف المصري، علي السيد الصواف
الخلاصـة: تناولت هذه الدراسة المستعرضة 1283 طفلاً من الأطفال الأصحّاء (681 ذكراً و602 أنثى) تـتـراوح أعمارهم بين 6 و11 عاماً، لدراسة التـرابط بين محيط الخصر وبين السِّمنة المركزية. وقد صُنِّفَ الأطفال وفقاً لمنسب كتلة الجسم إلى طبيعيـين ومفرطي الوزن وسِمَان. ولوحظ ترابط إيجابي مرتفع في كلا الجنسين بين محيط الخصر ومنسب كتلة الجسم، والنسبة المئوية للشحم في الجسم، وثخانة الطية الجلدية تحت لوح الكتف وفوق الحرقفة، ومجموع قياسات الطيات الجلدية. وكانت السِّمنة المركزية وفرط الوزن بسبب تـراكم الشحوم في مركز الجسم من المؤشرات على السِّمنة لدى كل من الأطفال الذكور والإناث الذين يعانون من السِّمنة، باستثناء من كان منهم في الفئة العمرية 6.5 ± 1 سنة. وكان محيط الخصر مؤشراً جيداً على السِّمنة المركزية (فرط الوزن والسِّمنة) في الأعمار التي تـتـراوح بين 8.5 ± 1 سنة و10.5 ± 1 سنة.
ABSTRACT: This cross-sectional study of 1283 healthy children (681 boys, 602 girls) aged 6–11 years tested the degree of correlation between waist circumference measurements and adiposity. The children were classified as normal, overweight or obese according to their body mass index (BMI). For both sexes a highly positive correlation was found between waist circumference and BMI, percentage of body fat, subscapular and suprailiac skinfold thicknesses, and the sum of skinfold measures. Central overweight and obesity were indicators for central fatness for both overweight boys and girls and for obese girls except in age group 6.5 ± 1 years. Waist circumference was a good indicator of central fatness (overweight and obesity) in children aged 8.5 ± years and 10.5 ± 1 years.
Tour de taille et adiposité centrale chez les enfants des écoles primaires en Égypte
RÉSUMÉ: Cette étude transversale réalisée auprès de 1283 enfants en bonne santé (681 garçons et 602 filles) âgés de 6 à 11 ans a permis d’évaluer le degré de corrélation entre les mesures du tour de taille et l’adiposité. Les enfants ont été classés comme normaux, en surpoids ou obèses en fonction de leur indice de masse corporelle (IMC). Pour les deux sexes, on a constaté une corrélation très positive entre le tour de taille et l’IMC, le pourcentage de tissu adipeux, l’épaisseur des plis cutanés sous-scapulaire et sus-iliaque, et la somme des mesures des plis cutanés. La surcharge pondérale et l’obésité centrales étaient des indicateurs d’adiposité centrale chez les garçons et les filles en surpoids et chez les filles obèses, sauf dans le groupe d’âge des 6,5 ± 1 ans. Le tour de taille était un bon indicateur d’adiposité centrale (surpoids et obésité) chez les enfants âgés de 8,5 ± 1 ans et de 10,5 ± 1 ans.
1Department of Biological Anthropology, National Research Centre, Dokki, Cairo, Egypt (Correspondence to S.A. El-Masry: This email address is being protected from spambots. You need JavaScript enabled to view it.)
Received: 13/12/05; accepted: 02/04/06
EMHJ, 2008,14(4):916-925
Introduction
Central fatness, mostly intra-abdominal fat, is medically more important than subcutaneous fat in the trunk. The ac-cumulation of both types of fat is affected by high food consumption and is therefore a historic novelty for human populations [1]. A central fat pattern has adverse health implications in both children and adults. Recent studies in children showed that a greater deposition of central fat correlates with less favourable patterns of serum lipoprotein concentrations, increased blood pressure [2], adverse levels of cardiovascu-lar risk [3] and increased risk of metabolic complications [4].
The ability of simple anthropometric techniques to correctly measure central adiposity needs to be assessed because adiposity tracks from childhood into adulthood [5]. Routine evaluation of regional fat distribution on a wide scale requires methods that are simpler than dual-energy X-ray absorptiometry (DXA), computerized tomography (CT) or magne-tic resonance imaging (MRI). However, studies on the efficacy of anthropometric techniques for identifying children with high central adiposity are scare. There is a suggestion that waist circumference alone may be a more useful and accurate tool in children than DXA etc. [6]. Taylor et al. found that waist circumference performed well in identifying children with high trunk fat as measured with DXA [5]. Waist circumference correctly identified > 90% of children as being true positives (high waist circumference and high trunk fat mass) or true negatives (low waist circumference and low trunk fat mass).
The circumference of the waist relates closely to body mass index (BMI) and is also the dominant measure in the waist-to-hip ratio, which reflects the proportion of the body fat located intra-abdominally, as opposed to subcutaneously [7]. The waist circumference is a better index of android (abdominal) obesity than waist-to-hip ratio and is the best indicator of changes in the intra-abdominal fat during weight loss [8]. Waist circumference independently contributes to the prediction of non-abdominal (total fat – abdominal fat), abdominal subcutaneous and visceral fat in both sexes. It has the ability to act as a surrogate for abdominal fat [9]. These observations reinforce the importance of using waist circumference in clinical practice [10].
We therefore believed that an exami-nation of waist circumference in a group of primary-school Egyptian children would add valuable comparative data to BMI data in assessment of central fatness in overweight and obese children. BMI is a poor proxy for central fatness [4] as it is an expression of weight not adiposity [11] and it provides no information on body fat distribution, so it can mask true obesity-related risk in children [3].
The aim of our study was to test the degree of correlation between waist circum-ference measurements of a sample of Egyptian schoolchildren with their adipo-sity (whether total or central), and to quan-tify the association of waist circumference measurements with age and degree of BMI (overweight or obese) in the same children.
Methods
Sample
This data were obtained from a cross-sectional survey of a sample of 1283 Egyptian schoolchildren, 681 boys and 602 girls, aged 6–11 years. The pupils were recruited from 2 public schools (El Zahraa primary school and El Orman El-Tagribia school) situated in Giza governorate, during the period October 2002 to April 2004. Permission to perform the study was granted by the Ministry of Education and the directors of the schools included in the research. Parents were informed about the purpose of the study and their permission (in the form of written consent) was obtained.
Data collection
The following was performed for each child:
A simple questionnaire was directed to the parents about personal abd socio-economic data (parental education and occupation, crowding index), the presence or absence of consanguinity, the medical history of the child with special emphasis on any chronic condi-tion or long-term systemic treatment. The socioeconomic status of the pupil was characterized by scoring parental education, occupation and crowding index as low (score 3–11), medium (12–16) and high (> 17). Only the medium-level pupils were enrolled in the study (the majority of the pupils in these 2 particular public schools).
Complete clinical examination to ex-clude organic and genetic disorders that might interfere with normal growth.
Anthropometric assessment was then made using standardized equipment, following the recommendations of the International Biological Program [12]. Three consecutive measurements were taken and when the difference between the readings was acceptable, the mean was recorded. Body weight was measured with minimal clothing (for which no cor-rection was made) using Seca scales and approximated to the nearest 0.01 kg. Height was measured without shoes using a Holtain portable anthropometer and approximated to the nearest 0.1 cm. Waist circumference was taken midway between the 10th rib and the top of the iliac crest (at the level of the umbilicus) using a flexible nonstretchable plastic tape and approximated to the nearest 0.1 cm. Subscapular and suprailiac skinfold thicknesses were measured on the left side of the body using Harpenden skinfold callipers and approximated to the nearest 0.2 mm. BMI (weight in kg/height2 in m) and the sum of the subscapular and suprailiac skinfold thicknesses (as an indicator of central adiposity) were calculated.
Each pupil was also examined by the Holtain Body Composition Analyser using bioelectrical impedance analysis to measure his/her body fat percentage (an estimate of the fraction of the total body mass that is adipose tissue) and percentage of lean using his/her age, weight and height approximated to the nearest unit.
The sample was classified into 3 age groups (6.5 ± 1, 8.5 ± 1 and 10.5 ± 1 years) for boys and girls. The limits proposed by the 2002 standard growth curves for Egyptian children and adolescents [133] were applied in reclassifying the sample according to BMI into normal (≥ 15% to < 85%), overweight (≥ 85% to < 95%) or obese (≥ 95%) according to the National Center for Health Statistics criteria [14]
Statistical analysis
Mean and standard deviation (SD) for all studied anthropometric measurements, indices and body fat percentage were calculated for each age and sex. Then the percentiles of waist circumference for overweight and obese children were estimated..
All the data were analysed using SPSS, version 9. The charts were drawn using Microsoft Excel software.
Results
The percentage of excess adiposity was nearly equal in girls and boys (12.2% of boys were overweight and 5.4% obese, while 11.8% of girls were overweight and 6.0% obese). Mean and SD for all the studied anthropometric measurements and the percentage of body fat by sex and age are presented in Table 1 and Table 2. Waist circumference was nearly equal between boys and girls at all ages, except at age 6.5 ± 1 years when girls recorded higher values than boys with no significant difference ((P > 0.05).
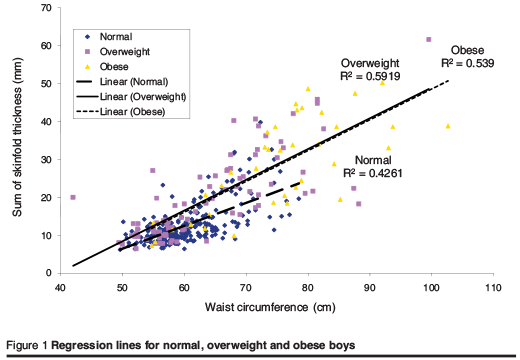
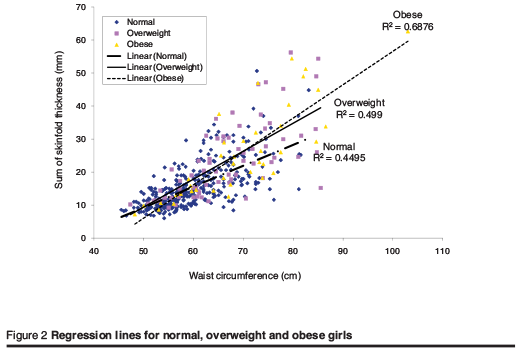
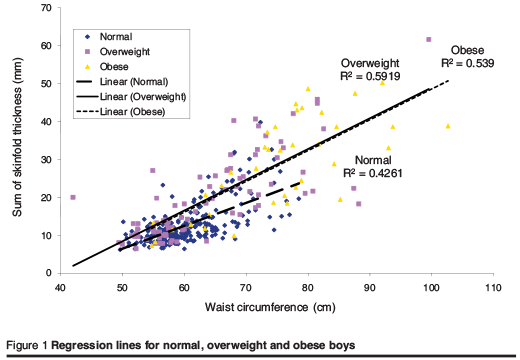
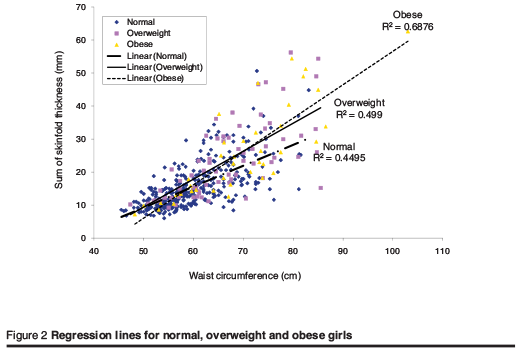
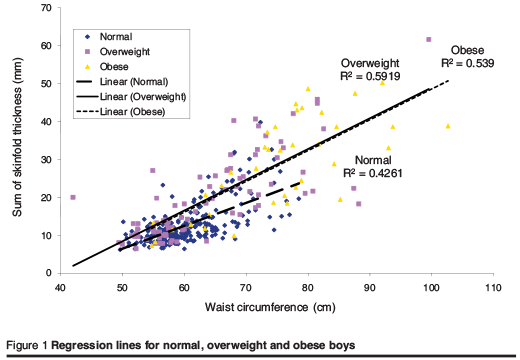
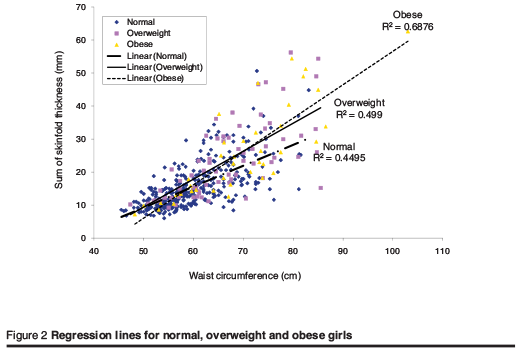
Table 3 ans Table 4 P < 0.0001). After adjustment for age, BMI, percentage body fat, subscapular and suprailiac skinfold thickness (Figure 1 and Figure 2), the sum of sub-scapular and supra-iliac skinfolds still had a high correlation with waist circumference in normal, overweight and obese pupils (RR2 = 0.43, 0.59 and 0.54 for boys and R2 = 0.45, 0.50 and 0.69 for girls, respectively).
Discussion
Central fatness in children is correlated with a less favourable metabolic profile [2]. Visceral fat or intra-abdominal adipose tissue (IAAT) can only be directly quantified with imaging techniques. IAAT has been detected in children as young as 5 years of age. IAAT generally increases in proportion with general fatness but the relationship between IAAT and total body fat is complex. In children, a major portion of the variance in IAAT is independent of total body fat. Central skinfold and waist circumference alone are highly correlated with IAAT as well as subcutaneous abdominal adipose tissue [166].
The definition of child overweight and obesity is arbitrary [16]. Comparison of our results regarding prevalence of overweight and obesity with another Egyptian study in Cairo [17] shows that they recorded higher values than our study (14.3% of boys and 13.8% of girls were overweight while 6.3% of boys and 6.7% of girls were obese). However they used BMI-for-age percentiles according to Hammer et al., not national reference standards, which might overestimate the real prevalence [18].
19]. Fernandez et al. described waist circumference percentiles of African–American, European–American and Mexican–American children and adolescents, and stated that waist circum-ference measurements increased in a mono-tonic fashion across ages but at non-constant rates and in a manner that varied with age and sex [[20].
Waist circumference was equal between boys and girls in all the studied age intervals except age 6.5 ± 1 years, when girls recorded higher values with no significant difference. However, Fredriks et al. found that mean waist circumference was slightly higher in boys than in girls and this difference was statistically significant from 11 years of age onwards among Dutch children [21]. The same was reported by Soar et al. among schoolchildren aged 7–9 years in Brazil [22].
In summary, we have shown that waist circumference correlates with total body fat percentage and BMI, and especially with central adiposity in the trunk region (central subcutaneous fat) in this age group of Egyptian primary-school children of both sexes in the 3 studied categories of BMI. Our results confirm the finding that waist circumference is a convenient measure of abdominal adipose tissue [23] and correlates closely with BMI [8,22], with centralized or upper body fat in young people [3,4,24] and with total body fat [25]. Taylor et al. also found in their study in New Zealand children aged 3–19 years that waist circumference performs well as an index of central adiposity in children and adolescents of both sexes over a wide age range [5].
Conclusions
Waist circumference is a good indicator for central fatness in children aged 8.5 ± 1 years and 10.5 ± 1 years. Waist circumference should be routinely measured in schoolchildren. Further work is necessary to examine the link between waist circumference, body fatness and morbidity in young people. National standards for waist circumference are needed to study trends in, and the likely medical and psychological costs of, obesity in young people.
References
- Lev-Ran A. Human obesity: an evolution--ary approach to understanding our bulging waistline. Diabetes/metabolism research and reviews, 2001, 17(5):347–62.
- Danials SR et al. Association of body fat distribution and cardiovascular risk factors in children and adolescents. Circulation, 1999, 99:541–5.
- McCarthy HD et al. Trends in waist circumferences in young British children: a comparative study. International journal of obesity and related metabolic disorders, 2005, 29(2):157–62.
- McCarthy HD, Ellis SM, Cole TJ. Central overweight and obesity in British youth aged 11–16 years: cross sectional sur-veys of waist circumference. British medical journal, 2003, 326:624–33.
- Taylor RW et al. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3–19 years. American journal of clinical nutrition, 2000, 72:490–5.
- Goran MI et al. Prediction of intra-abdominal and subcutaneous abdominal adipose tissue in healthy pre-pubertal children. International journal of obesity and related metabolic disorders, 1998, 22:549–58.
- Bjorntorp P. Classification of obese patients and complications related to the distribution of surplus fat. American journal of clinical nutrition, 1987, 45(Sup-pl. 5):1120–5.
- Kurpad SS, Tandon H, Srinivasan K. Waist circumference correlates better with body mass index than waist-to-hip ratio in Asian Indians. National medical journal of India, 2004, 17(2):115–6.
- Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Bestheda, Maryland, US Department of Health and Human Services, National Institutes of Health, 1998 (NHLBI document 98-4083).
- Janssen I et al. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous and visceral fat. American journal of clinical nutrition, 2002, 75:683–8.
- Zimmermann MB et al. Detection of overweight and obesity in a national sample of 6–12-y-old Swiss children: accuracy and validity of reference values for body mass index from the US Centers for Disease Control and Prevention and the International Obesity Task Force. American journal of clinical nutrition, 2004, 79:838–43.
- Hiernaux J, Tanner JM. Growth and physique: anthropometry. In: Weiner JS, Lourie JA, eds. Human biology, a guide to field methods. Philadelphia, FA Davis Company, 1969:2–42.
- Ghalli I et al. Standard growth curves for Egyptian children and adolescents 2002. Cairo, Egypt, Ministry of Health, 2002.
- National Center for Health Statistics in collaboration with the National Center for Chronic Disease Prevention and Health Promotion. Body mass index-for-age percentiles: boys, 2 to 20 years. Atlanta, Georgia, Centers for Disease Control and Prevention, 2000 (http://www.cdc.gov/nchs/data/nhanes/growthcharts/set2/chart%2015.pdf, accessed 9 October 2007).
- Goram MI. Visceral fat in prepubertal children: influence of obesity, anthropomet-ry, ethnicity, gender, diet, and growth. American journal of human biology, 1999, 11(2): 201–7.
- Cole TJ et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. British medical journal, 2000, 320:1240–53.
- Hafez AS, El-Awady MY, Hassan NE. Obesity profile among primary school children in Cairo. Egyptian journal of com-munity medicine, 2000, 18(1):99–119.
- Hammer LD et al Standardized percentile curves of body-mass index for children and adolescents. American journal of diseases of children, 1991, 145:259–63.
- McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0–16.9 y. European journal of clinical nutrition, 2001, 55(10):902–7.
- Fernández JR et al. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American child-ren and adolescents. Journal of pediatrics, 2004, 145(4):427–30.
- Fredriks AM et al. Are age references for waist circumference, hip circumference and waist-hip ratio in Dutch children useful in clinical practice? European journal of pediatrics, 2005, 164(4):216–22.
- Soar C, Vasconcelos FA, Assis MA. relação cintura quadril e o perímetro da cintura associados ao índice de massa corporal em estudo com escolares [Waist–hip ratio and waist circumference associated with body mass index in a study with school children]. Cadernos de saúde pública, 2004, 20(6):1609–16.
- Booth ML et al. The relationship between body mass index and waist circumfe-rence: implications for estimates of the population prevalence of overweight. International journal of obesity and related metabolic disorders, 2000, 24(8):1058–61.
- 24. Danials SR, Khourty PR, Morrison JA. Utility of different measures of body fat distribution in children and adolescents. American journal of epidemiology, 2000, 152:1179–84.
- Obesity: preventing and managing the global epidemic. Report of a WHO Consultation on Obesity, Geneva, 3–5 June. Geneva, World Health Organiza-tion, 1998 (WHO Technical Report Series, No. 894).
- Mueller WH, Kaplowitz HJ. The precision of anthropometric assessment of body fat distribution in children. Annals of human biology, 1994, 21(3):267–74
PDF version
N.E. Hassan,1 S.A. El-Masry1 and A.E. El-Sawaf1
محيط الخصر وتراكم الشحوم المركزي لدى الأطفال المصريـين في المدارس الابتدائية
نـيِّرة المرسي حسن، سحر عبد الرؤف المصري، علي السيد الصواف
الخلاصـة: تناولت هذه الدراسة المستعرضة 1283 طفلاً من الأطفال الأصحّاء (681 ذكراً و602 أنثى) تـتـراوح أعمارهم بين 6 و11 عاماً، لدراسة التـرابط بين محيط الخصر وبين السِّمنة المركزية. وقد صُنِّفَ الأطفال وفقاً لمنسب كتلة الجسم إلى طبيعيـين ومفرطي الوزن وسِمَان. ولوحظ ترابط إيجابي مرتفع في كلا الجنسين بين محيط الخصر ومنسب كتلة الجسم، والنسبة المئوية للشحم في الجسم، وثخانة الطية الجلدية تحت لوح الكتف وفوق الحرقفة، ومجموع قياسات الطيات الجلدية. وكانت السِّمنة المركزية وفرط الوزن بسبب تـراكم الشحوم في مركز الجسم من المؤشرات على السِّمنة لدى كل من الأطفال الذكور والإناث الذين يعانون من السِّمنة، باستثناء من كان منهم في الفئة العمرية 6.5 ± 1 سنة. وكان محيط الخصر مؤشراً جيداً على السِّمنة المركزية (فرط الوزن والسِّمنة) في الأعمار التي تـتـراوح بين 8.5 ± 1 سنة و10.5 ± 1 سنة.
ABSTRACT: This cross-sectional study of 1283 healthy children (681 boys, 602 girls) aged 6–11 years tested the degree of correlation between waist circumference measurements and adiposity. The children were classified as normal, overweight or obese according to their body mass index (BMI). For both sexes a highly positive correlation was found between waist circumference and BMI, percentage of body fat, subscapular and suprailiac skinfold thicknesses, and the sum of skinfold measures. Central overweight and obesity were indicators for central fatness for both overweight boys and girls and for obese girls except in age group 6.5 ± 1 years. Waist circumference was a good indicator of central fatness (overweight and obesity) in children aged 8.5 ± years and 10.5 ± 1 years.
Tour de taille et adiposité centrale chez les enfants des écoles primaires en Égypte
RÉSUMÉ: Cette étude transversale réalisée auprès de 1283 enfants en bonne santé (681 garçons et 602 filles) âgés de 6 à 11 ans a permis d’évaluer le degré de corrélation entre les mesures du tour de taille et l’adiposité. Les enfants ont été classés comme normaux, en surpoids ou obèses en fonction de leur indice de masse corporelle (IMC). Pour les deux sexes, on a constaté une corrélation très positive entre le tour de taille et l’IMC, le pourcentage de tissu adipeux, l’épaisseur des plis cutanés sous-scapulaire et sus-iliaque, et la somme des mesures des plis cutanés. La surcharge pondérale et l’obésité centrales étaient des indicateurs d’adiposité centrale chez les garçons et les filles en surpoids et chez les filles obèses, sauf dans le groupe d’âge des 6,5 ± 1 ans. Le tour de taille était un bon indicateur d’adiposité centrale (surpoids et obésité) chez les enfants âgés de 8,5 ± 1 ans et de 10,5 ± 1 ans.
1Department of Biological Anthropology, National Research Centre, Dokki, Cairo, Egypt (Correspondence to S.A. El-Masry: This email address is being protected from spambots. You need JavaScript enabled to view it.)
Received: 13/12/05; accepted: 02/04/06
EMHJ, 2008,14(4):916-925
Introduction
Central fatness, mostly intra-abdominal fat, is medically more important than subcutaneous fat in the trunk. The ac-cumulation of both types of fat is affected by high food consumption and is therefore a historic novelty for human populations [1]. A central fat pattern has adverse health implications in both children and adults. Recent studies in children showed that a greater deposition of central fat correlates with less favourable patterns of serum lipoprotein concentrations, increased blood pressure [2], adverse levels of cardiovascu-lar risk [3] and increased risk of metabolic complications [4].
The ability of simple anthropometric techniques to correctly measure central adiposity needs to be assessed because adiposity tracks from childhood into adulthood [5]. Routine evaluation of regional fat distribution on a wide scale requires methods that are simpler than dual-energy X-ray absorptiometry (DXA), computerized tomography (CT) or magne-tic resonance imaging (MRI). However, studies on the efficacy of anthropometric techniques for identifying children with high central adiposity are scare. There is a suggestion that waist circumference alone may be a more useful and accurate tool in children than DXA etc. [6]. Taylor et al. found that waist circumference performed well in identifying children with high trunk fat as measured with DXA [5]. Waist circumference correctly identified > 90% of children as being true positives (high waist circumference and high trunk fat mass) or true negatives (low waist circumference and low trunk fat mass).
The circumference of the waist relates closely to body mass index (BMI) and is also the dominant measure in the waist-to-hip ratio, which reflects the proportion of the body fat located intra-abdominally, as opposed to subcutaneously [7]. The waist circumference is a better index of android (abdominal) obesity than waist-to-hip ratio and is the best indicator of changes in the intra-abdominal fat during weight loss [8]. Waist circumference independently contributes to the prediction of non-abdominal (total fat – abdominal fat), abdominal subcutaneous and visceral fat in both sexes. It has the ability to act as a surrogate for abdominal fat [9]. These observations reinforce the importance of using waist circumference in clinical practice [10].
We therefore believed that an exami-nation of waist circumference in a group of primary-school Egyptian children would add valuable comparative data to BMI data in assessment of central fatness in overweight and obese children. BMI is a poor proxy for central fatness [4] as it is an expression of weight not adiposity [11] and it provides no information on body fat distribution, so it can mask true obesity-related risk in children [3].
The aim of our study was to test the degree of correlation between waist circum-ference measurements of a sample of Egyptian schoolchildren with their adipo-sity (whether total or central), and to quan-tify the association of waist circumference measurements with age and degree of BMI (overweight or obese) in the same children.
Methods
Sample
This data were obtained from a cross-sectional survey of a sample of 1283 Egyptian schoolchildren, 681 boys and 602 girls, aged 6–11 years. The pupils were recruited from 2 public schools (El Zahraa primary school and El Orman El-Tagribia school) situated in Giza governorate, during the period October 2002 to April 2004. Permission to perform the study was granted by the Ministry of Education and the directors of the schools included in the research. Parents were informed about the purpose of the study and their permission (in the form of written consent) was obtained.
Data collection
The following was performed for each child:
A simple questionnaire was directed to the parents about personal abd socio-economic data (parental education and occupation, crowding index), the presence or absence of consanguinity, the medical history of the child with special emphasis on any chronic condi-tion or long-term systemic treatment. The socioeconomic status of the pupil was characterized by scoring parental education, occupation and crowding index as low (score 3–11), medium (12–16) and high (> 17). Only the medium-level pupils were enrolled in the study (the majority of the pupils in these 2 particular public schools).
Complete clinical examination to ex-clude organic and genetic disorders that might interfere with normal growth.
Anthropometric assessment was then made using standardized equipment, following the recommendations of the International Biological Program [12]. Three consecutive measurements were taken and when the difference between the readings was acceptable, the mean was recorded. Body weight was measured with minimal clothing (for which no cor-rection was made) using Seca scales and approximated to the nearest 0.01 kg. Height was measured without shoes using a Holtain portable anthropometer and approximated to the nearest 0.1 cm. Waist circumference was taken midway between the 10th rib and the top of the iliac crest (at the level of the umbilicus) using a flexible nonstretchable plastic tape and approximated to the nearest 0.1 cm. Subscapular and suprailiac skinfold thicknesses were measured on the left side of the body using Harpenden skinfold callipers and approximated to the nearest 0.2 mm. BMI (weight in kg/height2 in m) and the sum of the subscapular and suprailiac skinfold thicknesses (as an indicator of central adiposity) were calculated.
Each pupil was also examined by the Holtain Body Composition Analyser using bioelectrical impedance analysis to measure his/her body fat percentage (an estimate of the fraction of the total body mass that is adipose tissue) and percentage of lean using his/her age, weight and height approximated to the nearest unit.
The sample was classified into 3 age groups (6.5 ± 1, 8.5 ± 1 and 10.5 ± 1 years) for boys and girls. The limits proposed by the 2002 standard growth curves for Egyptian children and adolescents [133] were applied in reclassifying the sample according to BMI into normal (≥ 15% to < 85%), overweight (≥ 85% to < 95%) or obese (≥ 95%) according to the National Center for Health Statistics criteria [14]
Statistical analysis
Mean and standard deviation (SD) for all studied anthropometric measurements, indices and body fat percentage were calculated for each age and sex. Then the percentiles of waist circumference for overweight and obese children were estimated..
All the data were analysed using SPSS, version 9. The charts were drawn using Microsoft Excel software.
Results
The percentage of excess adiposity was nearly equal in girls and boys (12.2% of boys were overweight and 5.4% obese, while 11.8% of girls were overweight and 6.0% obese). Mean and SD for all the studied anthropometric measurements and the percentage of body fat by sex and age are presented in Table 1 and Table 2. Waist circumference was nearly equal between boys and girls at all ages, except at age 6.5 ± 1 years when girls recorded higher values than boys with no significant difference ((P > 0.05).
Table 3 ans Table 4 P < 0.0001). After adjustment for age, BMI, percentage body fat, subscapular and suprailiac skinfold thickness (Figure 1 and Figure 2), the sum of sub-scapular and supra-iliac skinfolds still had a high correlation with waist circumference in normal, overweight and obese pupils (RR2 = 0.43, 0.59 and 0.54 for boys and R2 = 0.45, 0.50 and 0.69 for girls, respectively).
Discussion
Central fatness in children is correlated with a less favourable metabolic profile [2]. Visceral fat or intra-abdominal adipose tissue (IAAT) can only be directly quantified with imaging techniques. IAAT has been detected in children as young as 5 years of age. IAAT generally increases in proportion with general fatness but the relationship between IAAT and total body fat is complex. In children, a major portion of the variance in IAAT is independent of total body fat. Central skinfold and waist circumference alone are highly correlated with IAAT as well as subcutaneous abdominal adipose tissue [166].
The definition of child overweight and obesity is arbitrary [16]. Comparison of our results regarding prevalence of overweight and obesity with another Egyptian study in Cairo [17] shows that they recorded higher values than our study (14.3% of boys and 13.8% of girls were overweight while 6.3% of boys and 6.7% of girls were obese). However they used BMI-for-age percentiles according to Hammer et al., not national reference standards, which might overestimate the real prevalence [18].
19]. Fernandez et al. described waist circumference percentiles of African–American, European–American and Mexican–American children and adolescents, and stated that waist circum-ference measurements increased in a mono-tonic fashion across ages but at non-constant rates and in a manner that varied with age and sex [[20].
Waist circumference was equal between boys and girls in all the studied age intervals except age 6.5 ± 1 years, when girls recorded higher values with no significant difference. However, Fredriks et al. found that mean waist circumference was slightly higher in boys than in girls and this difference was statistically significant from 11 years of age onwards among Dutch children [21]. The same was reported by Soar et al. among schoolchildren aged 7–9 years in Brazil [22].
In summary, we have shown that waist circumference correlates with total body fat percentage and BMI, and especially with central adiposity in the trunk region (central subcutaneous fat) in this age group of Egyptian primary-school children of both sexes in the 3 studied categories of BMI. Our results confirm the finding that waist circumference is a convenient measure of abdominal adipose tissue [23] and correlates closely with BMI [8,22], with centralized or upper body fat in young people [3,4,24] and with total body fat [25]. Taylor et al. also found in their study in New Zealand children aged 3–19 years that waist circumference performs well as an index of central adiposity in children and adolescents of both sexes over a wide age range [5].
Conclusions
Waist circumference is a good indicator for central fatness in children aged 8.5 ± 1 years and 10.5 ± 1 years. Waist circumference should be routinely measured in schoolchildren. Further work is necessary to examine the link between waist circumference, body fatness and morbidity in young people. National standards for waist circumference are needed to study trends in, and the likely medical and psychological costs of, obesity in young people.
References
- Lev-Ran A. Human obesity: an evolution--ary approach to understanding our bulging waistline. Diabetes/metabolism research and reviews, 2001, 17(5):347–62.
- Danials SR et al. Association of body fat distribution and cardiovascular risk factors in children and adolescents. Circulation, 1999, 99:541–5.
- McCarthy HD et al. Trends in waist circumferences in young British children: a comparative study. International journal of obesity and related metabolic disorders, 2005, 29(2):157–62.
- McCarthy HD, Ellis SM, Cole TJ. Central overweight and obesity in British youth aged 11–16 years: cross sectional sur-veys of waist circumference. British medical journal, 2003, 326:624–33.
- Taylor RW et al. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3–19 years. American journal of clinical nutrition, 2000, 72:490–5.
- Goran MI et al. Prediction of intra-abdominal and subcutaneous abdominal adipose tissue in healthy pre-pubertal children. International journal of obesity and related metabolic disorders, 1998, 22:549–58.
- Bjorntorp P. Classification of obese patients and complications related to the distribution of surplus fat. American journal of clinical nutrition, 1987, 45(Sup-pl. 5):1120–5.
- Kurpad SS, Tandon H, Srinivasan K. Waist circumference correlates better with body mass index than waist-to-hip ratio in Asian Indians. National medical journal of India, 2004, 17(2):115–6.
- Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Bestheda, Maryland, US Department of Health and Human Services, National Institutes of Health, 1998 (NHLBI document 98-4083).
- Janssen I et al. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous and visceral fat. American journal of clinical nutrition, 2002, 75:683–8.
- Zimmermann MB et al. Detection of overweight and obesity in a national sample of 6–12-y-old Swiss children: accuracy and validity of reference values for body mass index from the US Centers for Disease Control and Prevention and the International Obesity Task Force. American journal of clinical nutrition, 2004, 79:838–43.
- Hiernaux J, Tanner JM. Growth and physique: anthropometry. In: Weiner JS, Lourie JA, eds. Human biology, a guide to field methods. Philadelphia, FA Davis Company, 1969:2–42.
- Ghalli I et al. Standard growth curves for Egyptian children and adolescents 2002. Cairo, Egypt, Ministry of Health, 2002.
- National Center for Health Statistics in collaboration with the National Center for Chronic Disease Prevention and Health Promotion. Body mass index-for-age percentiles: boys, 2 to 20 years. Atlanta, Georgia, Centers for Disease Control and Prevention, 2000 (http://www.cdc.gov/nchs/data/nhanes/growthcharts/set2/chart%2015.pdf, accessed 9 October 2007).
- Goram MI. Visceral fat in prepubertal children: influence of obesity, anthropomet-ry, ethnicity, gender, diet, and growth. American journal of human biology, 1999, 11(2): 201–7.
- Cole TJ et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. British medical journal, 2000, 320:1240–53.
- Hafez AS, El-Awady MY, Hassan NE. Obesity profile among primary school children in Cairo. Egyptian journal of com-munity medicine, 2000, 18(1):99–119.
- Hammer LD et al Standardized percentile curves of body-mass index for children and adolescents. American journal of diseases of children, 1991, 145:259–63.
- McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0–16.9 y. European journal of clinical nutrition, 2001, 55(10):902–7.
- Fernández JR et al. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American child-ren and adolescents. Journal of pediatrics, 2004, 145(4):427–30.
- Fredriks AM et al. Are age references for waist circumference, hip circumference and waist-hip ratio in Dutch children useful in clinical practice? European journal of pediatrics, 2005, 164(4):216–22.
- Soar C, Vasconcelos FA, Assis MA. relação cintura quadril e o perímetro da cintura associados ao índice de massa corporal em estudo com escolares [Waist–hip ratio and waist circumference associated with body mass index in a study with school children]. Cadernos de saúde pública, 2004, 20(6):1609–16.
- Booth ML et al. The relationship between body mass index and waist circumfe-rence: implications for estimates of the population prevalence of overweight. International journal of obesity and related metabolic disorders, 2000, 24(8):1058–61.
- 24. Danials SR, Khourty PR, Morrison JA. Utility of different measures of body fat distribution in children and adolescents. American journal of epidemiology, 2000, 152:1179–84.
- Obesity: preventing and managing the global epidemic. Report of a WHO Consultation on Obesity, Geneva, 3–5 June. Geneva, World Health Organiza-tion, 1998 (WHO Technical Report Series, No. 894).
- Mueller WH, Kaplowitz HJ. The precision of anthropometric assessment of body fat distribution in children. Annals of human biology, 1994, 21(3):267–74